CONTENTS
- Rapid Reference 🚀
- Groundwork:
- BiPAP & CPAP
- High flow nasal cannula (HFNC)
- Selecting which device to use
- Oxymizer
- Podcast
- Questions & discussion
- Pitfalls
general situations where noninvasive support doesn't work well
- Inadequate monitoring:
- The remainder of this chapter assumes that patients are receiving ICU-level monitoring, with immediate capability to intubate if needed. If this isn't the case, then these techniques may be less safe.
- Multiorgan failure:
- Noninvasive respiratory support is best suited to patients with isolated respiratory failure.
- For patients with multi-organ failure, these techniques are less likely to be successful (unless the cause of respiratory failure is very rapidly reversible).
indications for immediate intubation
- Examples of why a patient might need immediate intubation:
- Inability to protect airway.
- Cardiac arrest, severe multi-organ failure.
- Logistic considerations (e.g. patient needs procedures/scans which mandate intubation).
- Two scenarios where patients may look absolute terrible, yet do well without intubation:
- (1) Acute pulmonary edema (may turn around rapidly with BiPAP and high-dose nitroglycerine infusion).
- (2) Bronchospasm (asthma or COPD).
- When in doubt, a reasonable approach is often to support the patient on BiPAP while simultaneously preparing for intubation.
- If the patient responds well to BiPAP, then BiPAP may be continued.
- If the patient requires intubation, then the BiPAP will help pre-oxygenate prior to intubation.
The goal of noninvasive respiratory support is essentially to support the patient long enough for other therapies to work (e.g. antibiotics, bronchodilators, steroids). This may take a bit of time. As long as the patient is comfortable, protecting their airway, and stable/improving, that's OK.
appropriate goals for a patient receiving noninvasive respiratory support:
- Maintain adequate oxygenation.
- Provide adequate ventilatory support so that the patient is comfortable and doesn't develop respiratory muscle fatigue.
- Allow for secretion clearance, if that is an issue (e.g. in pneumonia).
- The patient should be able to protect their airway from aspiration.
- Serial clinical evaluation should show that the patient's condition is stable or improving.
inappropriate goals
- The patient must immediately improve.
- The ABG/VBG must immediately improve, or meet some arbitrary target (noting that such targets usually aren't evidence-based).
- Some retrospective studies demonstrate that failure of the blood gas to improve correlates with a requirement for intubation. However, such studies are generally confounded because clinicians are utilizing these very same blood gas values as an indication for intubation! Thus, circular logic creates to a self-fulfilling prophecy.
- The patient must be able to be weaned off noninvasive respiratory support within a few hours.
assessment of patient on noninvasive respiratory support

- Oxygenation should be adequate (e.g. >88%).
- If the patient has an reliable pulse oximetry waveform, this is the preferred assessment of oxygenation.
- To be clear: there are generally no advantages (and potentially some disadvantages) to using serial ABGs to assess oxygenation. ABGs should only be used if pulse oximetry is unreliable (e.g. due to a poor waveform or hemoglobinopathy).
- Work of breathing should be tolerable, and improved by noninvasive respiratory support.
- Respiratory rate trends are extremely useful.
- Other examination findings may reflect work of breathing (retractions, tri-podding, ability to speak in sentences, the patient's perception of their breathing).
- Global overall appearance (including mentation)
- How does the patient look?
- As long as the patient is mentating normally, their PaCO2 isn't profoundly elevated.
- When in doubt, frequent re-assessment will often clarify the patient's trajectory. Discussion with other team members (e.g. nurse and respiratory therapist) can help enormously.
- ABG/VBG?
- These are generally not needed. If the other parameters are reassuring (i.e. oxygenation, work of breathing, appearance, mentation), then an ABG/VBG is unnecessary. Alternatively, if the patient is deteriorating clinically, then a normal ABG shouldn't be reassuring.
- The main indication for blood gas analysis is if the patient's mental status is abnormal, but it's unclear whether mental status is altered due to hypercapnia or medication (e.g. patients receiving sedation to tolerate the BiPAP).
- Venous blood gas is entirely adequate in nearly all cases (unless the VBG oxygen saturation is incredibly low).

oronasal mask (often called “facial mask”)
- More commonly used interface in critical care.
- It does introduce a risk of aspiration if the patient vomits and is unable to remove the mask.
nasal mask
- Use of a nasal mask eliminates aspiration risk. However, air leak out of the mouth reduces the amount of ventilatory support provided.(10890620, 19050635)
- Overall, nasal masks seem to be less commonly used in critical care (and for the remainder of the discussion, “BiPAP” refers to the use of an oronasal mask).
- Nasal masks could potentially be an option for patients at high aspiration risk, especially if HFNC isn't available.
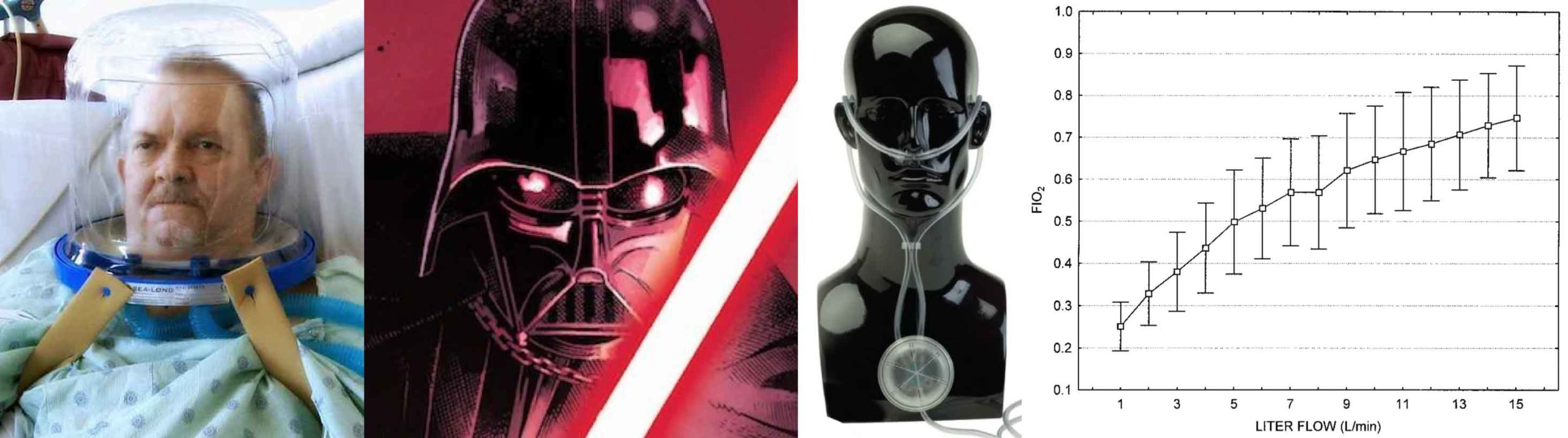
helmet
- This has several unique advantages:
- Easier to perceive facial expression & speak with the patient.
- Lower aspiration risk (vomitus may collect within the mask, but outside of the patient's airway).
- Lower risk of skin ulceration (avoids placing pressure over the bridge of the nose).
- Patients can drink liquids through a straw.
- Drawbacks:
- Noise exposure.
- Delayed triggering of the ventilator may reduce the mechanical support of breaths.
- One RCT of patients with ARDS found that the helmet interface reduced intubation rates and mortality rates. Unfortunately, the study was terminated early, leading to some controversy regarding these results.(27179847)
- Currently the helmet interface isn't widely available in the United States. Once this becomes available, it will be a useful tool to add to our noninvasive ventilatory support toolbox.
1) obvious contraindications
- Inability to tolerate the BiPAP mask (although sedation can sometimes help with this; see below).
- Anatomic barriers to mask seal (e.g. facial trauma or burns).
- Requirement for immediate intubation (e.g. cardiac arrest).
2) respiratory secretions
- BiPAP generally impairs expectoration, by reducing the pressure gradient which forces secretions out of the airway.
- BiPAP can be used for COPD patients with a mild amount of secretions (sometimes with intermittent breaks on HFNC, to allow for coughing and clearing secretions).
- BiPAP should be avoided for patients with copious secretions. In this situation, patients may initially improve on BiPAP, but eventually develop mucus plugging with subsequent deterioration.
3) aspiration risk (contraindication only for BiPAP via an orofacial mask)
- The risk of aspiration is a function of mental status and emesis risk:
- (a) Mental status: Patients with depressed mental status are at increased risk of aspirating. However, many patients with somnolence due to hypercapnia will do fine on BiPAP.
- (b) Emesis risk:
- i) Active or recent vomiting is probably the strongest risk factor.
- ii) Gastrointestinal pathology may increase risk of emesis (e.g. pancreatitis, bowel obstruction, gastrointestinal hemorrhage).
- iii) Gastric distension on imaging studies (including point-of-care ultrasonography) could conceivably be used to gauge risk.
strongest evidence: Heart failure & COPD
- RCTs on patients with heart failure and COPD have shown that BiPAP reduces intubation rates and mortality among sicker patients.
- The benefit is greatest among sicker patients (e.g. COPD patients with pH < 7.30).
- It's unclear whether patients with more mild disease would also benefit from BiPAP (e.g. in a COPD patient with normal pH yet severe dyspnea). Currently, this is a clinical determination made at the bedside, based largely on patient appearance.
- In heart failure, CPAP is as effective as BiPAP.
- Heart failure and COPD are somewhat unique in this chapter, as situations where there is a definitive front-line therapy. Of course, not all patients will respond favorably to noninvasive ventilation. Occasional patients with COPD or heart failure may do better with HFNC, but in general BiPAP should be front line therapy (especially in the sickest patients).
asthma
- The physiology of asthma is often similar to COPD, although the two diseases aren't identical (with each disease containing various phenotypes).
- Asthmatics may have acute bronchospasm as a primary problem.
- COPD patients often have greater problems with diaphragmatic fatigue.
- There is fairly compelling evidence to support the use of noninvasive respiratory failure in asthma. Overall, there is a growing consensus that noninvasive ventilation is a front-line therapy here (with persistent controversy regarding which pressures to use).
- For more, see the asthma chapter.
diaphragm-workload mismatch
- In some situations, the primary problem is a mismatch between the mechanical load on the diaphragm versus the strength of the diaphragm. For example:
- (1) Obesity hypoventilation syndrome: Normal diaphragm versus increased work of breathing.
- (2) Neuromuscular weakness (e.g. muscular dystrophy): Weak diaphragm versus a normal work of breathing.
- BiPAP provides the greatest amount of mechanical support for the work of breathing. Therefore, BiPAP might theoretically be a front-line therapy in these conditions. However, most of the evidence here pertains to chronic nocturnal BiPAP, rather than using BiPAP for acute respiratory failure.
This may be worthwhile for patients with a highly BiPAP-responsive disease process (section above). In other situations, it may be wise to transition to HFNC if there are difficulties tolerating BiPAP.
dexmedetomidine
- Often a first-line sedative to allow tolerance of BiPAP within the ICU. Possibly the agent with the greatest amount of evidentiary support.(24577019, 24683260, 22975538)
- Advantages: titratable agent, doesn't suppress respiratory drive.
- Disadvantages:
- Gradual onset (a loading bolus is generally avoided, as this may cause marked hemodynamic instability).
- May cause bradycardia and hypotension.
- Limited availability.
IV droperidol or haloperidol
- Advantages:
- Hemodynamically stable.
- Don't suppress respiratory drive.
- Widely available (haloperidol particularly, although the availability of droperidol is improving).
- Reasonably rapid onset (roughly 5-15 minutes).
- Some anti-emetic properties as a bonus.
- Disadvantages:
- Cannot be immediately down-titrated (if the patient becomes over-sedated, this will last for a while).
- May prolong QT and cause Torsades de Pointes (but the risk is extraordinarily low at the doses used for mild sedation).
- When provided via an intravenous route, both drugs are fairly similar. Haloperidol seems to be roughly half as potent as droperidol, but haloperidol can achieve similar clinical effects when dosed appropriately.
- The primary advantage of droperidol over haloperidol seems to be faster onset when given via an intra-muscular route.
IV ketamine dissociation (e.g. >1-1.5 mg/kg bolus)
- Advantages:
- Achieves immediate behavioral control and sedation.
- Hemodynamically stable.
- Doesn't suppress respiration.
- Disadvantages:
- Short-term solution (patients will wake up within ~30-60 minutes).
- Some risk of emesis as patients emerge from sedation.
- Overall, ketamine is useful for patients who are truly crashing (and thus unable to wait long enough to use another agent). This isn't a long-term sedation solution, but rather a bridge to another strategy, for example:
- (1) Ketamine dissociation, patient improves on BiPAP –> re-evaluate, consider initiation of dexmedetomidine or droperidol as needed.
- (2) Ketamine dissociation, patient fails to respond to BiPAP –> intubation.
- Further information: Delayed sequence intubation (DSI).
IV fentanyl (or other opioid)
- Effects:
- (1) It will reduce the respiratory rate – which can be helpful for patients with marked tachypnea (if the tachypnea and increased work of breathing are themselves detrimental).
- (2) It may provide some sedative effects.
- Possibly useful in the following situations:
- (1) Asthma or COPD with marked tachypnea (may reduce respiratory rate, allowing for more effective exhalation).
- (2) Pneumonia with marked tachypnea (reduction in respiratory rate may prevent the patient from tiring out).
- (3) Any situation where the patient has severe air hunger that is leading to dyssynchrony or flow starvation on noninvasive ventilation (the BiPAP or CPAP cannot provide a fast enough flow to satisfy the patient).
- Disadvantages
- (1) It can cause hypercapnia and hypoventilation.
- (2) With opioids on board, a reduction in respiratory rate isn't necessarily indicative of clinical improvement – so this makes it harder to assess the patient.
- Cautions!
- It should be used only by practitioners who are skilled in the management of respiratory failure, and also with intensive monitoring.
- Some mode of ventilatory monitoring should be employed in patients receiving opioids (e.g. monitoring of tidal volumes and minute ventilation on the BiPAP machine).
- Further information:
- Rationale for using opioids to brake the respiratory drive here.
- Use of opioid in asthma: point & counterpoint.
benzodiazepines
- These are widely used, but probably aren't the best agents (unless the patient was previously on benzodiazepines and is known to respond favorably to them).
- Drawbacks to benzodiazepines:
- (1) Tendency to cause delirium.
- (2) May cause paradoxical agitation.
- (3) Unpredictable dose-response curve.
- One small RCT comparing midazolam versus dexmedetomidine found that midazolam increased the risk of intubation.(22975538)
continuous positive airway pressure (CPAP)
- This very simply provides a continuous level of positive airway pressure (analogous to PEEP on a ventilator).
- CPAP is useful in situations where all you need is to increase the airway pressure:
- (1) For heart failure, CPAP is as effective as BiPAP. CPAP will reduce preload and afterload, exerting a physiologic effect which is similar to an ACE inhibitor.
- (2) CPAP might conceivably be useful in patients with compressive atelectasis, where you're trying to increase the mean airway pressure as much as possible to maximize lung recruitment.
bilevel positive airway pressure (BiPAP or BPAP)
- This provides the following:
- (1) A baseline level of positive pressure at all times (the expiratory Positive Airway Pressure, or ePAP).
- (2) An increase in the pressure when the patient triggers a breath (the inspiratory Positive Airway Pressure, or iPAP).
- BiPAP is analogous to pressure support mode on a mechanical ventilator. The patient determines the respiratory rate, the length of each breath, and the flow rate.
- This is the most widely used mode of noninvasive support.
- Technically, “BPAP” is the most proper term for this mode (since “BiPAP” was originally used as a trade-name by Respironics). However, nobody really cares. This chapter uses the term BiPAP, because BiPAP is the most commonly used term in clinical practice.
modes which include ventilator-triggered breaths
- Occasionally, modes may be used which include ventilator-triggered breaths (sometimes referred to as a “backup rate”).
- Ventilator-triggered breaths may be volume-cycled or pressure-cycled (as with an invasive ventilator).
- The use of ventilator-triggered breaths in acute respiratory failure is somewhat questionable. If the patient is so sick that they aren't generating a reliable respiratory rate, they probably ought to be intubated.
- Potential indications to use ventilator-triggered breaths:
- (a) Very sick patients who are unwilling to be intubated (DNI).
- (b) Patients with central sleep apnea, who benefit from chronic use of nocturnal noninvasive ventilation with ventilator-triggered breaths.
- (c) Ventilator-triggered breaths are excellent for supporting respiration during the apneic period of rapid sequence intubation (more on this here).
limits of inspiratory pressure
- Increasing the pressure may increase the risk of gas insufflation into the gastrointestinal tract, increasing the risk of aspiration.
- The exact pressure at which aspiration risk increases is unclear, but this probably occurs around 20 cm. (24317204) Consequently, it may be wise to avoid inspiratory pressures above ~20 cm.
 setting BiPAP for congestive heart failure
setting BiPAP for congestive heart failure
- Expiratory pressure (ePAP) is the key here. A high ePAP will maintain high intrathoracic pressures throughout the respiratory cycle, which will off-load the heart.
- Example:
- Start at 10 cm inspiratory pressure / 5 cm expiratory pressure (allowing the patient to get used to the mask).
- Increase to 15 cm inspiratory pressure / 10 cm expiratory pressure.
- Increase to 18 cm inspiratory pressure / 15 cm expiratory pressure.
- CPAP is also perfectly fine and is equally effective.
setting BiPAP for neuromuscular weakness (e.g. myasthenia gravis)
- The key here is the difference between the inhaled pressure and the exhaled pressure. This is the “driving pressure” which provides mechanical support for each breath.
- Example:
- Start at 10 cm inspiratory pressure / 5 cm expiratory pressure.
- Increase to 15 cm inspiratory pressure / 5 cm expiratory pressure.
- Increase to 18 cm inspiratory pressure / 5 cm expiratory pressure.
COPD/Asthma
- BiPAP achieves two things for these patients:
- The ePAP balances out AutoPEEP (positive pressure due to gas trapping in the patient's lungs). This makes it easier for patients to take each breath.
- The driving pressure (inhaled pressure – exhaled pressure) provides support for each new breath.
- Example:
- Start at 10 cm inspiratory pressure / 5 cm expiratory pressure.
- Increase to 15 cm inspiratory pressure / 8 cm expiratory pressure.
- Increase to 18cm inspiratory pressure / 8 cm expiratory pressure.
- The optimal strategy for setting BiPAP is unknown (and in all likelihood, no universally applicable strategy exists). The best approach is titration at the bedside, depending on the patient's comfort and tidal volumes.
“black box” ventilator
- These are devices which are designed for outpatient therapy of sleep apnea or obesity hypoventilation syndrome.
- These are not preferred for treatment of acute respiratory failure, for the following reasons:
- (1) They lack any graphical display of the patient's respiratory behavior.
- (2) Some may be unable to generate high flow rates (leaving the ventilator unable to provide enough support for a very dyspneic patient).
full mechanical ventilator
- These are standard mechanical ventilators, designed for use with intubated patients.
- These are a major improvement compared to the “black box” ventilator (for example, they can provide graphics and fast flow rates).
- Depending on the device, they may not compensate well for gas leaks around the mask.
ventilator designed for BiPAP
- A purpose-designed ventilator specifically intended for BiPAP may be the best option in many situations.
- These devices are designed specifically to optimize both breath triggering and leak compensation.

background: low-flow devices
- “Low-flow” devices include a standard nasal cannula, venturi mask (“venti mask”), or non-rebreather face-mask (“NRB”). Low-flow devices have the following drawbacks:
- (1) They can deliver only up to ~60% FiO2 (even a “100% non-rebreather facemask” provides only ~60% FiO2).
- (2) They don't provide full heating and humidification (which is potentially uncomfortable).
- (3) They can't provide precisely titrated amounts of FiO2. If the patient is breathing rapidly, the patient will inhale air from around the mask, thereby reducing the inhaled FiO2.
- If HFNC is available, then HFNC is generally superior to venturi masks or non-rebreather face-masks (especially for prolonged respiratory support).
what is HFNC?
- HFNC involves generation of warmed, humidified air which is then delivered via nasal cannula at flow rates up to ~70 liters/minute.
- Patients can usually tolerate high flow rates because the gas is heated and humidified (otherwise this is very uncomfortable).
- Fresh gas will typically fill the patient's oropharynx (thus, the upper airway may function analogously to a non-rebreather reservoir).
- HFNC achieves three things:
- (1) This will deliver an inspired FiO2 which is fairly close to the set FiO2. For example, a HFNC set at 100% FiO2 can provide substantially more oxygen than any low-flow device (providing nearly 100% FiO2).
- (2) The high flow rate may provide a little positive pressure in the upper airway (similar to PEEP).
- (3) Washout of carbon dioxide in the upper pharynx reduces the work of breathing via dead space washout…
what is dead space washout?
- Dead space is the volume of gas which is moved in and out of the airway, but doesn't participate in CO2 clearance from the blood.
- Dead space is detrimental to the patient because the patient has to expend work to move this gas, but it provides no effective ventilation.
- Dead space can generally be divided into alveolar and anatomic components:
- Anatomic dead space is the volume of the upper airways (extending from the mouth to the respiratory bronchioles). This is roughly equal in ml to the patient's weight in pounds (e.g. an average-sized 170 pound person may have 170 ml anatomic dead space).
- Alveolar dead space is gas which gets into the alveoli, but doesn't participate in gas exchange (e.g. due to lung disease such as ARDS).
- HFNC jets fresh gas into the nose and upper pharynx, which reduces the anatomic dead space.
- Normally the anatomic dead space extends from the respiratory bronchioles to the mouth (the site of fresh gas exchange).
- With HFNC, the anatomic dead space extends from the respiratory bronchioles to only the mid-tracheal level (since fresh gas is being pumped into the upper airway).
- By reducing the anatomic dead space, HFNC makes ventilation more efficient. This allows the patient to achieve the same amount of CO2 clearance while moving less gas into their lungs, which reduces the work of breathing.
general properties of HFNC
- Generally well tolerated.
- No significant contraindications (other than obvious ones, such as bilateral nasal packing). This allows HFNC to be used in situations where BiPAP may be contraindicated (e.g. patients at high risk of emesis).
- No real risks (aside from potentially delaying intubation).
- Can be continued for prolonged periods of time (unlike BiPAP, which eventually causes nasal ulceration).
- Allows patients to eat.
- Allows unimpaired ability to communicate (facilitating patient assessment).
- Provides powerful support of oxygenation (with up to 100% FiO2 and some PEEP).
- Provides some support of ventilation (due to washout of dead space).
use of HFNC
- Can be widely applied, to a variety of disease processes. For example, there's probably no form of respiratory failure which wouldn't derive some benefit from HFNC (when compared to low-flow oxygen).
- Of course, in many cases this amount of benefit might be small and thus clinically insignificant.
- HFNC is arguably front-line therapy for patients with parenchymal lung disease (e.g. pneumonia or interstitial lung disease).
- The FLORALI trial found superior outcomes with HFNC compared to BiPAP for patients with acute lung injury (predominantly due to pneumonia)
flow rate
- Main consequences of higher flow rate:
- i) Greater dead space washout – which may translate into a reduction in the work of breathing.
- ii) Increased PEEP (but this is a fairly minimal effect).
- The usual range of flow rate is ~20-60 liters/minute.
- How to titrate flow rate:
- i) Flow rate is titrated predominantly against the patient's work of breathing (e.g. respiratory rate).
- ii) For patients with refractory hypoxemia, increasing the flow could theoretically increase the oxygenation a wee bit (due to PEEP).
- For patients who are in acute respiratory failure and doing poorly, it may be helpful to increase the flow rate as high as the patient will tolerate (e.g. 60 liters/minute)
FiO2
- May be adjusted between 21%-100%.
- This is titrated against oxygen saturation.
- There is no need to check an ABG to measure the pO2, if the patient has a functioning pulse oximeter (more on this here).
weaning off HFNC
- If the patient can be weaned down to 20 liters/minute flow at 50% FiO2, then they may be ready to tolerate a nasal cannula at 6 liters/minute.
- When in doubt, empiricism is king here: empirically trial the low-flow nasal cannula.
- Note that a standard nasal cannula at 6 liters/minute can provide ~40-50% FiO2, so patients may be ready to transition to a low-flow cannula earlier than may be obvious.
how is this done?
- Using a standard nasal cannula, increase the flow rate to 15 liters/minute. Then give the flowmeter about a half dozen rotations to increase the flow even higher. You're aiming for a flow rate of roughly ~25-35 liters/minute.
- That's all. This can be instituted within seconds, using any nasal cannulae and any flowmeter.
what does this achieve?
- High-flow nasal cannula mimic: This is essentially a STAT high-flow nasal cannula that will provide the patient with a lot of oxygen. Around 30 liters/minute of 100% oxygen will achieve an inhaled oxygen of ~90% with some degree CO2 washout.
- Nasal irritation: Providing cold, non-humidified oxygen will be irritating and uncomfortable for the patient. If the patient is obtunded and dying, then some mild stimulation is often a good thing (to stimulate an endogenous sympathetic response). If the patient is fully conscious, reassure them that this is a temporary intervention that will only last a few minutes.
is this safe?
- Commercial high-flow nasal cannula devices deliver up to 70 liters/minute flow to the nose, so we know that 70 liters/minute flow is safe. It's unclear what the maximal safe rate is (80? 90?).
- The flow rate is not precisely monitored with this technique (that's why it's dirty) – but you shouldn't be getting anywhere close to >70 liters/minute flow.
- Some flowmeters have a maximal flow rate (figure below), which could provide some additional reassurance. (However, note that you're never going to come close to maxing out the flowmeter.)
when should dirty high flow be used?
- This is merely intended as a temporary stop-gap measure to provide high levels of oxygen for a crashing patient, when other devices aren't immediately available.
- Examples of situations where this may be useful:
- Patient starts precipitously desaturating during bronchoscopy.
- Any patient whose saturation abruptly plummets to dangerously low levels (e.g., to provide high-level oxygen support during the minute it takes to set up a bag-valve mask).
- Preoxygenation prior to crash intubation (this isn't the preferred modality of preoxygenation prior to intubation, but it can be helpful if staff and materials are limited). 🌊
treat emergent pleural disease with drainage
- Severe pleural disease can cause frank respiratory failure. Examples of this include:
- (1) Tension pneumothorax.
- (2) Massive pleural effusion (which can also cause a tension phenomenon – although this is less common than tension pneumothorax).
- Patients with acute respiratory failure due to pleural disease require emergent pleural drainage. This is obviously true for pneumothorax, but often gets overlooked in patients with pleural effusions.
upper airway obstruction can be temporized with Heliox
- Heliox is a mixture of helium and oxygen which has reduced viscosity compared to air or oxygen. This is a nice temporizing measure for patients with upper airway obstruction (e.g. stridor). Heliox will often reduce their work of breathing substantially.
- Examples of the use of Heliox:
- Post-extubation laryngeal edema often will improve over a period of hours with the use of steroid and racemic epinephrine. Heliox may be used as a bridge towards recovery, avoiding intubation.
- For a patient with undifferentiated stridor, Heliox may be used to buy time while obtaining materials and colleagues needed for definitive management (e.g. nasolaryngoscopy, intubation with a double-setup).
- Heliox is available only in fixed ratios (typically containing 60%-70% Helium and 30-40% FiO2). Therefore, Heliox cannot be used for a patient with significant hypoxemia who requires >40% FiO2.
avoid BiPAP or HFNC for primary CNS disease
- A very common error is to try to treat a patient with drug intoxication (e.g. opioids) with BiPAP. This isn't appropriate or safe.
- If the patient is so intoxicated that respiratory support is needed, then antidotal therapy is indicated (e.g. naloxone). If this fails, the patient should be intubated.
- Note that patients with mild hypercarbia who are protecting their airway don't necessarily require any respiratory support at all! The goal is not for the patient to have a normal PaCO2 (see “goals” above).
 This is a general cognitive rubric for how to select different devices. However, the following points should be stressed:
This is a general cognitive rubric for how to select different devices. However, the following points should be stressed:
- Large randomized trials may not apply perfectly to the unique patient in front of you (e.g. there are considerable inter-individual variations, for example regarding claustrophobia and secretion volume).
- When in doubt, the key is close monitoring while trialing various devices. It's impossible to predict exactly how any specific patient will respond to a given therapy.
- Please note that arterial blood gas values aren't needed to determine which device to use. The key to device selection is the underlying diagnosis.
 basics
basics
- Oxymizers might be the best-kept secret of respiratory therapy.
- This is essentially a nasal cannula with a built-in oxygen reservoir. While the patient is exhaling, oxygen flowing from the tank will accumulate in the oxygen reservoir. When the patient inhales, they entrain this accumulated bolus of oxygen from the reservoir. Overall, this leads to a more efficient transfer of oxygen to the patient, thereby achieving a higher effective FiO2.
- For any given flow rate (e.g. 2 liters/minute), the oxymizer will increase the FiO2 which the patient experiences.
- Various designs are available as shown above. They work similarly, with marked differences in fashion:
- A mustache-style device is sometimes preferred for inpatients, as this reminds providers that the patient is on an oxymizer.
- The oxymizer pendant is more stylish for outpatient wear.
use of an oxymizer?
- The primary use is for patients with chronic hypoxemic respiratory failure.
- i) An oxymizer may reduce the flow rate of oxygen needed (so patients don't require as many oxygen canisters for trips).
- ii) For severe hypoxemic respiratory failure, an oxymizer may be the only way to achieve an adequate oxygen saturation using a nasal cannula.
Follow us on iTunes
The Podcast Episode
Want to Download the Episode?
Right Click Here and Choose Save-As
To keep this page small and fast, questions & discussion about this post can be found on another page here.

- The goal of noninvasive respiratory support isn't necessarily to improve the ABG values, it is to reduce the work of breathing and improve patient comfort (thereby avoiding respiratory exhaustion). Focus on the patient, not the ABG!
- In order to be effective, all of these techniques must be applied early in the course of respiratory failure (before the patient has developed severe diaphragmatic fatigue).
- Don't use BiPAP blindly in any patient with hypercarbia. The underlying diagnosis is more important than the ABG values in determining how to treat the patient.
Guide to emoji hyperlinks 
= Link to online calculator.
= Link to Medscape monograph about a drug.
= Link to IBCC section about a drug.
= Link to IBCC section covering that topic.
= Link to FOAMed site with related information.
= Link to supplemental media.
References
- 10890620 Navalesi P, Fanfulla F, Frigerio P, Gregoretti C, Nava S. Physiologic evaluation of noninvasive mechanical ventilation delivered with three types of masks in patients with chronic hypercapnic respiratory failure. Crit Care Med. 2000 Jun;28(6):1785-90. doi: 10.1097/00003246-200006000-00015 [PubMed]
- 19050635 Girault C, Briel A, Benichou J, Hellot MF, Dachraoui F, Tamion F, Bonmarchand G. Interface strategy during noninvasive positive pressure ventilation for hypercapnic acute respiratory failure. Crit Care Med. 2009 Jan;37(1):124-31. doi: 10.1097/CCM.0b013e3181928706 [PubMed]
- 22975538 Huang Z, Chen YS, Yang ZL, Liu JY. Dexmedetomidine versus midazolam for the sedation of patients with non-invasive ventilation failure. Intern Med. 2012;51(17):2299-305. doi: 10.2169/internalmedicine.51.7810 [PubMed]
- 24317204 Bouvet L, Albert ML, Augris C, Boselli E, Ecochard R, Rabilloud M, Chassard D, Allaouchiche B. Real-time detection of gastric insufflation related to facemask pressure-controlled ventilation using ultrasonography of the antrum and epigastric auscultation in nonparalyzed patients: a prospective, randomized, double-blind study. Anesthesiology. 2014 Feb;120(2):326-34. doi: 10.1097/ALN.0000000000000094 [PubMed]
- 24577019 Devlin JW, Al-Qadheeb NS, Chi A, Roberts RJ, Qawi I, Garpestad E, Hill NS. Efficacy and safety of early dexmedetomidine during noninvasive ventilation for patients with acute respiratory failure: a randomized, double-blind, placebo-controlled pilot study. Chest. 2014 Jun;145(6):1204-1212. doi: 10.1378/chest.13-1448 [PubMed]
- 24683260 Senoglu N, Oksuz H, Dogan Z, Yildiz H, Demirkiran H, Ekerbicer H. Sedation during noninvasive mechanical ventilation with dexmedetomidine or midazolam: A randomized, double-blind, prospective study. Curr Ther Res Clin Exp. 2010 Jun;71(3):141-53. doi: 10.1016/j.curtheres.2010.06.003 [PubMed]
- 27179847 Patel BK, Wolfe KS, Pohlman AS, Hall JB, Kress JP. Effect of Noninvasive Ventilation Delivered by Helmet vs Face Mask on the Rate of Endotracheal Intubation in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA. 2016 Jun 14;315(22):2435-41. doi: 10.1001/jama.2016.6338. PMID: 27179847; PMCID: PMC4967560 [PubMed]