The Enemy of Good is Perfect
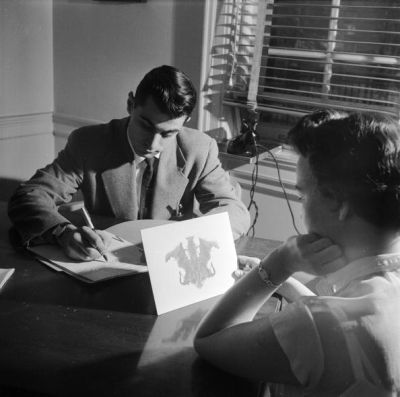
The interpretation of literature is not dissimilar from the interpretation of the Rorschach tests. To one person the data appears to be a freshly hatched butterfly full of hope and promise. While to another it is a discomforting stain resulting from the splatter of improperly handled bodily excrement. What you see when looking at the data is based less on the strength of the trial in question and more on your own intrinsic biases. This psycho-statistical phenomenon has never been more true than with anti-arrhythmic medications in cardiac arrest. Those that believe in their efficacy cling strongly to their potential physiological benefits and data from two small RCTs demonstrating an increase in survival to hospital admission in patients who received amiodarone vs placebo or lidocaine (1,2). Those of us who are bent more towards nihilism discard these findings as surrogate endpoints which do not translate into patient oriented survival. Despite being the largest study examining this question, enrolling over 4,000 patients, I fear that the ALPS trial will do nothing to change these conflicting opinions.
Published in the NEJM on April 4th 2016, Kudenchuck et al examined 3026 patients in refractory ventricular fibrillation or pulseless ventricular tachycardia, randomly assigned to receive either amiodarone, lidocaine or placebo (3). Patients were enrolled if they were found to be in a shockable rhythm which was resistant to at least one attempt at electrical defibrillation and the use of vasoactive agents. Patients were administered either 300 mg of amiodarone, 120 mg of lidocaine, or 3 ml of a saline-based placebo. If further attempts at defibrillation were unsuccessful paramedics were permitted to administer a second bolus at half the dose of the first.
The authors found survival to hospital discharge (their primary endpoint) varied little between groups (24.4%, 23.7% and 21% respectively). This 3.2% and 2.6% absolute difference in survival between the amiodarone vs placebo, and lidocaine vs placebo failed to reach statistical significance (p= 0.08 and 0.16 respectively). The author did note that despite their statistical failure, both amiodarone and lidocaine demonstrated signs of efficacy. Patients randomized to either the amiodarone or lidocaine arms received less defibrillation attempts before achieving ROSC (5, 5, 6 respectively) and survived to hospital admission (45.7%, 47% 39% respectively) more frequently than patient randomized to the placebo arm. In the subset of patients whose arrest was witnessed by bystanders, the authors report a statistically significant increase in patients discharged from the hospital alive in both the amiodarone and lidocaine group when compared to placebo (27.7%, 28.7% and 22.7% respectively) (3).
Some will argue that amiodarone and lidocaine’s benefits were hidden behind a statistically insignificant p-value due in part to a misjudgment in the power calculation. This very well may be true. Certainly patients in both the amiodarone and lidocaine groups seem to respond to the antiarrhythmic effects of the drug therapy. But these upstream benefits did not translate into neurologically intact survival. Survival with good neurological outcome (mRS ?3) was 18.8%, 17.5% and 16.6% respectively (3). More importantly since their primary endpoint failed to reach statistical significance, it is equally reasonable to argue that these trends towards benefit occurred simply by chance alone. That these small improvements in prehospital outcomes were a measure of a prognostically healthier population rather than an effect of the lidocaine or amiodarone. It is not hard to imagine that patients who survive to hospital admission more frequently and require less shocks are the same patients who are more likely to have improved neurological survival.
But let us suppose for a moment that the trends observed in the ALPS Trial describe a true benefit in the treatment of refractory ventricular fibrillation in OHCA. To what end? The authors primary endpoint was based off a per-protocol analysis of their cohort. As such they excluded a large portion of patients (1,627) because on retrospective analysis their initial rhythms were not ventricular fibrillation or pulseless ventricular tachycardia (3). This led to a highly select population, intended to optimize the trials ability to discern benefit for the treatments in question. But such an analysis comes at a cost of its external validity. Even in this artificial population the authors found only small trends to improvement in survival and had to perform further subgroup analysis to demonstrate statistical benefit. In fact, when the intention to treat population is examined even these trends towards improved survival all but disappear. Patient randomized to the amiodarone, lidocaine, placebo group had survived to hospital discharge at a rate of 19%, 18.4%, and17.6% respectively (3). What this means is for the overwhelming majority of patients in cardiac arrest with a shockable rhythm, amiodarone or lidocaine will provide no benefit.
One could argue that despite the overall minimal effect, these drugs should be administered to all comers on the rare chance they may help one individual patient. And this position seems reasonable when viewed from this single perspective. But when each of these low yield, ineffective therapeutic strategies are stacked one on top of another, on top of another on top of another, the resulting system is unwieldy and ineffective. Cardiac arrest is a high acuity, time dependent disease state. We should focus on delivering a small number of high yield interventions in a timely fashion. Continued attention on interventions which are unable to demonstrate statistically meaningful improvements in neurological outcomes in over 3,000 patients does nothing but add cognitive clutter to an already chaotic milieu.
This trial design does not account for the unintended consequences of adding extraneous and ineffective complexities to your resuscitation strategy. Trials like the OPALS and the Olasveengen et al cohort which examine the value of ACLS, when added to CPR and rapid defibrillation, demonstrated that such resuscitative intricacies provide no additional survival benefits to patients (4,5).
While the administration of of either amiodarone or lidocaine will likely have little effect on patient outcomes, it is important not to lose sight of the bigger picture. Our current strategy in the management of sudden cardiac arrest is to regain a perfusing rhythm through the application of CPR and rapid defibrillation. Every trial that has ever shown benefit in patient survival focused on the efficient deployment of these two interventions. So often high quality chest compressions, rapid rhythm analysis, avoiding perishock pauses and overzealous ventilatory strategies are overlooked in favor of accommodating the proper order of ACLS medications (6). The false Dichotomy Fallacy is better known by the phrase, the enemy of good is perfect. By creating a system that attempts to account for every last cause of cardiac arrest no matter how unlikely, regardless of the impotency of our resulting treatments, we create a system that is perfect in every way except that it is cumbersome and ineffective. A system that serves only to distract from the select few interventions that truly matter.
Sources Cited:
- Kudenchuk PJ,Cobb LA, Copass MK, et al. Amiodarone for resuscitation after out-of-hospital cardiac arrest due to ventricular fibrillation. N Engl J Med 1999;341:871-878
- Dorian P,Cass D, Schwartz B, Cooper R, Gelaznikas R, Barr A. Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. N Engl J Med 2002;346:884-890
- Kudenchuk PJ, Brown SP, Daya M, et al. Amiodarone, lidocaine, or placebo in out-of-hospital cardiac arrest. N Engl J Med. DOI: 1056/NEJMoa1514204
- Stiell IG, Wells GA, Field B, et al. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med. 2004;351(7):647-56.
- Olasveengen TM, Sunde K, Brunborg C, Thowsen J, Steen PA, Wik L. Intravenous drug administration during out-of-hospital cardiac arrest: a randomized trial. JAMA. 2009;302(20):2222-9.
- Gray R, Iyanaga M, Wang HE. Decreases in basic life support chest compression fraction after advanced life support arrival. Resuscitation. 2012;83(11):e208-9.
- EM Nerd-The Case of the Partial Cohort - May 24, 2020
- EM Nerd: The Case of the Sour Remedy Continues - January 20, 2020
- EM Nerd-The Case of the Adjacent Contradictions - December 23, 2019
Strongly agree with your general comment on CA management. Perfect is a way to far from good outcome in CA. I just think that PEA (in particular pseudo-PEA) and traumatic CA are different stories and deserve different consideration about searching for reversible causes and their management. In those cases we have to review our usually few good things to do, prioritising other interventions. In thise cases probably a “perfect” expertise is better than every protocol.
Really interested about your opinion.
Thanks
Mario Rugna
Hi Mario, Thanks for the comments. I completely agree, the management of PEA is completely different. It seems the majority of PEA arrest are due to agonal rhythms. So either a V-fib/V-tach that has been down to long and either spontaneously converted or was defibrillated into a PEA rhythm or a massive MI causing massive cardiac dysfunction. As such it is typically a poor prognostic sign. Certainly in the Bobrow cohort, the the patients with PEA arrest did worse when CCR was initiated. Likely this was due to the few respiratory arrests that needed airway management or an indicator that… Read more »