CONTENTS
- Rapid Reference 🚀
- Diagnosis
- Treatment
- Podcast
- Questions & discussion
- Pitfalls
Salicylate intoxication checklist ✅
Labs & targets (cycle q2hr until resolution) 📖
- Glucose: Target >80-100 mg/dL if altered mental status.
- Potassium: Target >4-4.5 mEq/L.
- Serum pH: Target ~7.5-7.55
- Urine pH: Target ≧7.5
- Salicylate level: Cycle until <40 mg/dL (<2.9 mM).
Consider glucose for abnormal mental status 📖
- Brain glucose levels may be low despite adequate serum levels.
- Give D50 empirically for patients with altered mental status.
Volume resuscitation 📖
- Confirm with echo, but in general patients are usually quite volume depleted.
- pH <7.5 Use isotonic bicarbonate as a resuscitative fluid (150 mEq/L in D5W).
- pH >7.5 Use balanced crystalloid (e.g. Lactated Ringers or Plasmalyte).
- DO NOT give normal saline (this worsens acidosis).
Alkalinization 📖
- Indicated if salicylate >40 mg/dL (>2.9 mM) and/or symptoms (i.e., most significant intoxications)
- Start with 2-3 amps (50 mEq each) of bicarb given as a slow push over ~10 min.
- Follow with isotonic bicarbonate (150 mEq/L) as maintenance fluid at ~200 ml/hr.
- Aggressively replete potassium to maintain >4-4.5 mEq/L (it will drop).
- Target serum pH 7.5-7.55 & urine pH ≧7.5
Hemodialysis indications 📖
- (1) Altered mental status or pulmonary edema.
- (2) pH <7.2 despite bicarbonate.
- (3) Salicylate >100 mg/dL (7.2 mM).
- (4) Salicylate >90 mg/dL (6.5 mM) with renal dysfunction, or despite fluid resuscitation/alkalinization.
- (5) Salicylate >80 mg/dL (5.8 mM) with renal dysfunction and despite fluid resuscitation/alkalinization.
- ⚠️ If any doubt exists, call nephrology & poison control for help early & often.
sources of salicylate
- Aspirin (lethal dose is really low (~150 mg/kg or ~10-30 grams). That's as few as 30 tablets of 325-mg aspirin.
- Many over-the-counter combination medications contain aspirin.
- Bismuth subsalicylate (Pepto-bismol).
- Topical products (e.g. Bengay, wart removers).
typical clinical presentations
- (1) Suicide attempt.
- (2) Inadvertent overdose in patients chronically using aspirin (often elderly with multiple medical problems).
signs & symptoms
- General:
- Tachypnea.
- Tachycardia.
- Diaphoresis.
- Hyperthermia.
- Neurologic:
- Tinnitus, vertigo, ataxia, deafness.
- Delirium, agitation, lethargy.
- Seizure, coma.
- GI:
- Nausea/vomiting.
- Diarrhea.
- Can cause gastritis with hematemesis.
- Pulmonary:
- Non-cardiogenic pulmonary edema.
acid-base abnormalities
- Acid-base status can suggest salicylate toxicity, but cannot exclude it. Note also that patients with co-ingestion may not manifest with classic acid/base patterns (e.g., aspirin plus opioids may not lead to a respiratory alkalosis). Nonetheless, the classic pattern of findings is as follows:
- (1) First finding is respiratory alkalosis.
- Salicylate affects the medulla directly, increasing respiratory drive.
- (2) Second, an anion-gap metabolic acidosis develops as well, creating a mixed picture.
- Metabolic acidosis reflects increases in ketoacid, salicylic acid, and lactic acid.
- Most of the elevated anion gap is not due to salicylate itself (<5 mM contribution).(32579814)
- (3) Respiratory acidosis may rarely occur.
- This is often a pre-terminal event (reflecting respiratory exhaustion, ARDS, or severe CNS dysfunction).
- Respiratory acidosis frequently occurs with co-ingestion of substances that reduce respiratory drive.
- Regardless of the etiology, this is very scary because these patients aren't defending their pH. Acidemia promotes entry of salicylate into the brain, worsening the intoxication. This creates the possibility of a death spiral involving hypercapnia, acidosis, and CNS dysfunction:
salicylate level – rough benchmarks
- 15-30 mg/dL (1-2.2 mM): Therapeutic.
- >40-50 mg/dL (>2.9-3.6 mM): Intoxication in most patients.
- >80-100 mg/dL (>5.7-7.2): Scary high, dialysis may be indicated.📖
limitations of salicylate levels
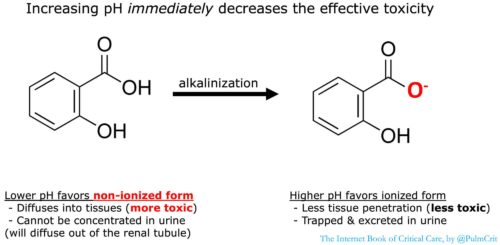
- (1) Variability in pH
- Harm is primarily caused by the non-ionized form of salicylate (figure below). The non-ionized salicylate level depends on both the total salicylate level and the pH (non-ionized salicylate level is increased by acidemia). For example, a patient with pH 7.2 and a total salicylate level of 46 mg/dL has the same level of nonionized salicylate as another patient with a pH of 7.55 and a total salicylate level of 100 mg/dL (figure below).
- (2) Acute vs. chronic intoxication
- In chronic intoxication the serum levels may underestimate the severity of the intoxication, because salicylate has already accumulated in the brain.
- Patients with chronic intoxication may have only slightly elevated levels, or even levels that fall into the “therapeutic” range.(32579814)
- (3) Timing of levels
- Levels usually peak around six hours after ingestion. However, the peak may be delayed for >12 hours in patients who have ingested enteric coated tablets.
avoid intubation
- Avoid or delay intubation if possible. Intubation may be extremely dangerous for patients with combined metabolic acidosis and respiratory alkalosis. In this scenario, hypoventilation may eliminate respiratory compensation, causing the pH to drop. This may push patients into the Salicylate Hypercapnia-Acidosis Death Spiral (figure above).
- Indications for intubation might include:
- Frank loss of airway protection with active vomiting or ongoing seizures.
- Hypercapnia (unlike most patients who are hyperventilating, intubation should improve pH in these patients).
- For patients who don't need intubation, high-flow nasal cannula may help blow off CO2 and reduce the work of breathing.
- However, HFNC should be discontinued as the serum bicarbonate levels rise to avoid excessive alkalemia.
- If intubation is necessary, risk may be reduced by:
- (a) Giving bicarbonate before intubation (2 mEq/kg bolus of hypertonic bicarbonate). This should be done >5-10 minutes before paralysis, so that the patient has time to blow off excess CO2 from the infused bicarbonate.
- (b) Intubation should be done rapidly by the most experienced staff available.
- (c) After intubation, immediately connect the patient to a ventilator and adjust settings to maximize minute ventilation (e.g., 8-10 cc/kg breaths, increase rate as high as possible without causing autoPEEP). Once the metabolic acidosis is controlled (over several hours), ventilator settings should be titrated down.
decontamination
- If patient is intubated and aspirin ingestion was within 1 hour, administer activated charcoal.
- If not intubated, don't give charcoal. (This is controversial, these patients have a tendency to lose their mental status and vomit.)
- Whole bowel irrigation could be considered for an intubated patient who consumed a large amount of enteric-coated tablets.
glucose
- CNS glucose levels are often lower than the blood level.
- Glucose should be given to patients with altered mental status, even if their serum glucose levels are normal (e.g., 1-2 ampules of D50W).
- The target glucose level is unclear, but it may be reasonable to maintain the glucose >80-100 mg/dL (>4.4-5.5 mM).
- Glucose infusion should be considered in severe intoxication. Most patients will receive an infusion of isotonic bicarbonate which is formulated in D5W, which should suffice.
goals
- (1) Reduce penetration of salicylate into the tissues (especially the brain).
- This is still beneficial, even in patients with anuric renal failure.
- (2) Increase excretion of salicylate in the urine.
indications for alkalinization
- Salicylate level >40 mg/dL (>2.9 mM).
- All symptomatic patients.
- Note: even if blood pH is already alkalemic due to respiratory alkalosis (pH up to 7.55), bicarbonate may still be beneficial to achieve urinary alkalinization.
general technique
- Start with a loading dose of 1-2 mEq/kg of hypertonic sodium bicarbonate.
- A typical ampule of bicarbonate in the United States is 50 mEq in 50 ml (1 mEq/ml). So 1-2 mEq/kg equates to ~2-3 ampules of hypertonic bicarbonate.
- Run a maintenance infusion of isotonic bicarbonate at ~200 ml/hr (D5W with three ampules of bicarbonate per liter to create a 150 mEq/L solution of sodium bicarbonate).
- Dextrose in this solution is beneficial to increase brain glucose levels (discussed above).
- Titrate based on chemistries.
- Stop alkalinization when salicylate levels fall below toxic levels (<40 mg/dL or <2.9 mM).
manipulation of urine pH
- Acetazolamide should not be used to directly alkalinize the urine.
- Acetazolamide use runs the risk of lowering serum pH. Additionally, the acetazolamide may displace salicylate from protein binding, thereby increasing plasma free salicylate levels.(32579814)
- If sufficient bicarbonate is administered, the kidneys should eventually excrete it leading to urinary alkalinization.
- Two measures are needed to achieve urinary alkalinization:
- (1) Euvolemia (hypovolemia will tend to cause increased renal bicarbonate reabsorption)
- (2) Potassium should be repleted aggressively (when the kidney retains potassium it does this by secreting acid into the urine). Isotonic bicarbonate tends to drop the potassium, so preemptive potassium repletion helps stay ahead of this.
monitoring
- Check serum pH q2hr, target pH ~7.5-7.55.
- Target a urine pH of at least 7.5
- Target potassium level >4.5 mM.
volume resuscitation
- Patients are generally substantially volume depleted for many reasons (diaphoresis, tachypnea, nausea/vomiting, diarrhea). Total body fluid deficit may commonly be 4-6 liters.(19641282)
- Patients should be volume resuscitated, with a goal of establishing euvolemia.
- Exception/caution: Avoid large volume fluid if patient already has pulmonary edema.
- The preferred fluid for volume resuscitation depends on the patient's pH:
- For patients with pH <7.5, isotonic bicarbonate may be used for both volume resuscitation and alkalization.
- For patients who are at target pH (7.5-7.55), lactated ringers (LR) or plasmalyte may be used for volume resuscitation.
- DO NOT give normal saline for resuscitation, as this will lower pH and potentially aggravate the intoxication.
general philosophy on dialysis
- Hemodialysis is extremely effective in salicylate intoxication. In severe salicylate intoxication, dialysis may be life-saving.
- Dialysis often takes several hours to set up. Therefore, for patients who are deteriorating clinically, it is often wise to initiate dialysis early. The risks of performing hemodialysis early (under controlled settings) are far lower than the risks of a severe salicylate intoxication (ICU mortality of 15%!).
- Unless you're putting in the dialysis catheter with a hacksaw or your nephrologist is inebriated, dialysis is safer than the natural history of severe salicylate intoxication.
- Clinical status is an important factor in the decision to dialyze. When in doubt, careful attention to the patient with serial evaluations may be helpful.
- Serial neurologic examination may be the best single reflection of real-time salicylate levels in the tissue (“end-organ” effect).
indications for dialysis per EXTRIP guidelines
- (1) Altered mental status or noncardiogenic pulmonary edema
- (2) Noncardiogenic pulmonary edema requiring supplemental oxygen
- (3) Salicylate level
- >100 mg/dL (7.2 mM)
- >90 mg/dL (6.5 mM) with renal dysfunction
- >90 mg/dL (6.5 mM) despite supportive care (e.g. fluid resuscitation)
- > 80 mg/dL (5.8 mM) despite supportive care and in context of renal dysfunction
- (4) pH < 7.2 despite supportive care (e.g. bicarbonate)
- Volume overload which prevents adequate alkalization is a potential indication for dialysis
- The key summary table from the EXTRIP guidelines is below. 📄
 intermittent hemodialysis preferred
intermittent hemodialysis preferred
- Intermittent hemodialysis is preferred over continuous renal replacement, because it is more efficient.
- Intermittent hemodialysis is recommended even in the context of hypotension. Since fluid isn't being removed, there is no evidence that hemodialysis causes more hemodynamic instability than continuous renal replacement therapy.
rebounding salicylate levels
- Hemodialysis will typically drop the blood salicylate levels dramatically. However, levels may rebound following cessation of dialysis.
- Follow salicylate levels and clinical symptoms following dialysis. In some cases, multiple dialysis runs may be necessary.
- Cycle labs at least q2hr initially.
- Glucose: Target moderate hyperglycemia.
- Electrolytes: Target potassium > 4.5 mM
- Alkalinization if patient has symptoms or a salicylate level >40 mg/dL (2.9 mM)
- Serum pH: target 7.5-7.55
- Urine pH: target >7.5
- Salicylate level.
- Creatinine kinase (rhabdomyolysis can occur).
Serum alkalization can be stopped when the following criteria are met:
- Two levels show that the salicylate level is consistently decreasing.
- Salicylate level <40 mg/dL (<2.9 mM).
- Patient is asymptomatic with a normal respiratory rate.
Following discontinuation of alkalinization, it may be reasonable to follow labs for 2-4 additional hours to ensure that acidosis doesn't recur (especially in chronic toxicity).
Follow us on iTunes
The Podcast Episode
Want to Download the Episode?
Right Click Here and Choose Save-As
To keep this page small and fast, questions & discussion about this post can be found on another page here.
- Without a suggestive history, salicylate intoxication can be extremely difficult to diagnose (e.g., sepsis mimic).
- When in doubt, it may be best to err on the side of early dialysis.
- Call nephrology early and often. For patients who are deteriorating, advocate for early dialysis. I'm often skeptical about dialysis for intoxication (e.g. for lithium), but early dialysis is key for severe salicylate intoxication.
- Avoid intubation if possible.
- Don't give normal saline (may lower the pH, worsening intoxication).
Guide to emoji hyperlinks 
= Link to online calculator.
= Link to Medscape monograph about a drug.
= Link to IBCC section about a drug.
= Link to IBCC section covering that topic.
= Link to FOAMed site with related information.
- 📄 = Link to open-access journal article.
= Link to supplemental media.
References
- 19641282 Pearlman BL, Gambhir R. Salicylate intoxication: a clinical review. Postgrad Med. 2009 Jul;121(4):162-8. doi: 10.3810/pgm.2009.07.2041 [PubMed]
- 25986310 Juurlink DN, Gosselin S, Kielstein JT, Ghannoum M, Lavergne V, Nolin TD, Hoffman RS; EXTRIP Workgroup. Extracorporeal Treatment for Salicylate Poisoning: Systematic Review and Recommendations From the EXTRIP Workgroup. Ann Emerg Med. 2015 Aug;66(2):165-81. doi: 10.1016/j.annemergmed.2015.03.031 [PubMed]
- 32579814 Palmer BF, Clegg DJ. Salicylate Toxicity. N Engl J Med. 2020 Jun 25;382(26):2544-2555. doi: 10.1056/NEJMra2010852 [PubMed]