I've been waiting for this one for a long time. I get to interview Dr. Stephen Bernard on the topic of post-arrest care.
Professor Stephen Bernard
 Senior Intensivist, The Alfred Hospital
Senior Intensivist, The Alfred Hospital
Professor Stephen Bernard is a senior Intensive Care Physician at the Alfred Hospital and Director of Intensive Care at Knox Private Hospital in Victoria, Australia. He is also Medical Advisor to Ambulance Victoria.
Last Week, I posted Part I of this interview on Post-Arrest Care 2013
This is Part II.
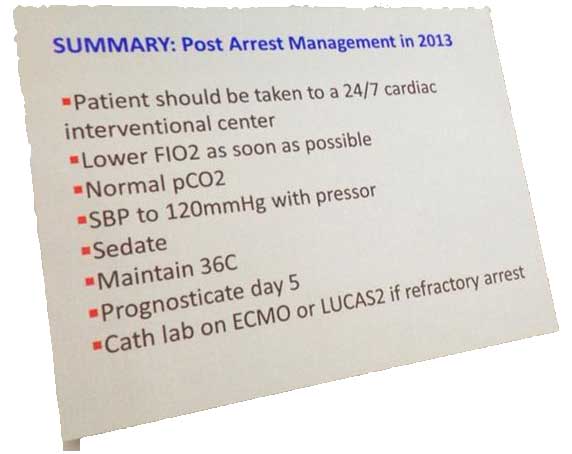
My discussion with Dr. Bernard was based on a talk he gave at the Australasian College for Emergency Medicine
MAP Goals
SBP of 120 mm hg? The paper was just published ahead-of-print
The other paper Dr. Bernard Mentioned is Gaieski et al. (Resuscitation 2007;73:29-39)
Sedate
If cooling to 36, it is a lot easier to get away with standard sedation practice as the hypothermia-slowed metabolism is no longer a big problem
Cath lab with ECMO or LUCAS2 for refractory arrest
It can be done! And if we can do it, is “stay-and-play” on scene still a good strategy?
CHEER trial (CPR, Hypothermia, ECMO and Early Reperfusion)
15 F arterial cath and a 17-19 F venous catheter under ultrasound guidance, with the only pause during compressions being the initial vessel puncture and 1st wire advancement
Intraarrest Hypothermia?
The animal data look good, but need human trials that show benefit. If you do it, then these patients may need a deeper degree of hypothermia (33 C?).
Prehospital Hypothermia and is Quicker Better?
Dr. Bernard's trial did not show benefit for prehospital cooling [cite source='pubmed']20679551[/cite]
and the in-press study by Kim et al. showed the same [cite source='pubmed']24240712[/cite]
More from Steve can be found at the EDECMO Podcast Site
Additional New Information
More on EMCrit
Additional Resources
You Need an EMCrit Membership to see this content. Login here if you already have one.
- EMCrit 373 – Mike Weinstock with another Critical Care Bounceback: “Asymptomatic Hypertension” - April 18, 2024
- EMCrit Wee – Ross Prager on 10 Heuristics for the New ICU Attending - April 13, 2024
- EMCrit 372 – FoundStab Intubation SOP - April 5, 2024
can one do a cath with lucas on the patient operating? wouldnt that get in the way of the flouro?
http://www.dicardiology.com/article/cath-lab-staff-saves-lives-impossible-cases-lucas-2-chest-compression-system
In my hospital we use auto pulse for cath lab PCI/cpr. This is band system rather than a plunger, it works well.
Hi Scott My apologies, this is the third time I am posting this as the criteria for prognostication got cut out of the last two posts. I’ve deleted possibly offending formatting in this one. Please delete the other two posts or people will think I am a broken record. Great podcast as usual. However there are two points regarding prognostication that I want to discuss – timing and necessary tests. Prior to therapeutic hypothermia this was an area of great clinical certainty (maybe the only one in medicine!) The American Academy of Neurology published a guideline in 2006 (Wijdicks, Neurology,… Read more »
Not sure we can say that Greg. Eelco’s paper was predicated on pts without targeted temp management. 36 is still mild hypothermia and the best evidence we have right now is the TTM Paper protocol. Would be easy for the authors to look at the 36 group retrospectively and compare the Wijdick’s recs vs. their own protocol to see if there is agreement. Worth an email to the authors by you.
Man, now you folks are just coming up with reasons for us medics to not have any fun 🙂
(I’m kidding.)
Great topic to have listened to, especially since prehospital post-ROSC protocols tend to be a little generic (if the system even HAS one). I’m interested to see what impact PCI with ECMO/LUCAS will have, particularly for more rural EMS services. Traditionally, cardiac arrest has been a no-go for our airmedical folks….I wonder if some further development of who benefits most from the mCPR/PCI approach will change things.
: ) We’ll have to bring some other cool stuff out to the field to make up for it.
Brilliant series of podcasts, Scott. These have been particularly interesting for us pre-hospital folk and found myself thinking of several cases where transport under CPR to receive ECMO at ED may have made significant differences. I’m wondering if open cardiac surgery is something that is/could be undertaken with an appropriate history? The case I have in mind is a 16 y/o whom remained in PEA after non-traumatic catastrophic valve failure (history of valve defect). The use of mechanical CPR devices is also very exciting, especially for patient transport. Several colleagues were injured in a crash this year whilst transporting a… Read more »
Hey Andy,
Yes a blown valve is a great case for ecmo. Pt has a reversible condition and should have good function after operative repair.
As to cpr in the back of a moving bus, it is super-dangerous as you say. I want my medics seatbelted in as the bus is barreling through traffic.
Scott, Wondering if you would be willing to speculate on why TTM study targeted mild/minimal hypothermia 36C instead of simply avoidance of fever, perhaps targeting 37C? Only talking about 37C) with antipyretics and no cooling? TTM study did not have third arm targeting normothermia. Maybe 33C, 36C and 37C with other advances in post-arrest care would all have same outcome? If you could, I would also love to hear your thoughts on the use of portable ECLS/ECMO in the ED. Would be interested whether you see small, portable ECMO/ECLS (extra-corporeal life support) devices as currently or on the horizon having… Read more »
Sorry about typo, meant to say: “(Only talking about <1C from normotheric 37C)"
Scott,
You might want to listen to this podcast. As to the temp choice, the surprise is not that they chose 36 instead of 37, but instead 36 instead of 35. 35 (and now 36) seems to be the temp where we get ICP reduction, fever prevention, and less side effects.
Hi Scott – I took your suggestion and wrote to Niklas Neilsen a while ago, he just got back to me saying that he has forwarded my question to the group neurologist. I’ll update you when I hear back from him.
Hi,
I see that Steve Bernard recommends shooting for a systolic BP of 120. What he doesn’t say is how to get there. In a patient who is hypotensive post ROSC (assuming no STEMI), what inotrope/pressor would you reach for first?
Thanks,
Jo