 CONTENTS
CONTENTS
- Venous injection of contrast (e.g. for CT scan)
- Intra-arterial contrast (e.g. cardiac catheterization)
- Algorithm
- Podcast
- Questions & discussion
- Pitfalls

The concept of contrast nephropathy was born in the 1950's, when it was observed that some patients developed renal failure following injection of IV contrast dye for intravenous pyelography.(13217726) This might have represented a true nephrotoxic reaction. The contrast dye used at that time probably was poisonous (50% diodone, a high-osmolar contrast dye which nobody would imagine using today). However, none of these early studies had adequate control groups, so it's impossible to know for sure. This was before the establishment of evidence-based medicine.
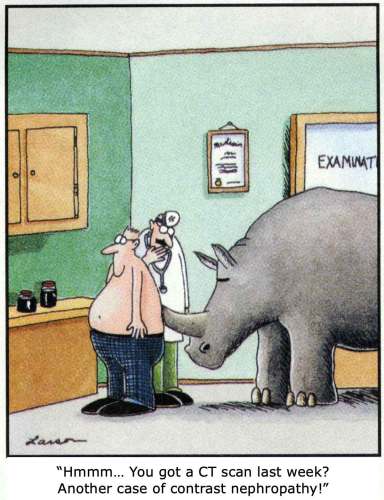
Regardless, a myth was born. Over time, fear of contrast nephropathy blossomed and took root. Any renal failure which occurred following the administration of contrast was likely to be labeled as “contrast nephropathy.” Over the ensuing decades, well over a thousand publications were written about contrast nephropathy.
Older contrast dyes probably were nephrotoxic. However, modern contrast dyes (with lower osmolarity) don't seem to cause renal failure.
“Contrast nephropathy” is usually defined as a small increase in creatinine within the days following contrast administration (e.g. 0.3 mg/dL). The assumption driving this is that even small bumps in creatinine reflect genuine renal damage, which in turn is clinically relevant. However, upon closer examination, this chain of reasoning doesn't hold up…
(1) does contrast dye cause an increase in creatinine?
Unfortunately, it would be unethical to perform a prospective RCT to evaluate this. Consequently, we are limited to retrospective, propensity-matched studies (which attempt to eliminate confounding variables). Recently, numerous studies and meta-analyses have emerged which don't detect any relationship between contrast dye administration and elevation of creatinine.(23319662, 24475854,23360742, 28131489, 30798098, 28197679, 28811122, 24656402, 20651198, 25203000, 30480553)
One clever study examined creatinine changes in patients who had received both a contrasted CT scan and also a non-contrasted CT scan at different points in time.(23360742) Changes in creatinine following both scans were the same, regardless of whether the patient had received a contrasted or non-contrasted CT scan. This demonstrates that creatinine levels normally bounce a certain amount. If we examine only creatinine elevations and assume that these represent “contrast nephropathy,” then we may manufacture a disease – when in fact we are looking at random statistical noise.
Indeed, several studies have found that the average creatinine of a group of patients exposed to IV contrast doesn't change at all.(24656402, 20707658, 17317065, 25183538) Some patients experience an increase in creatinine, while an equal number experience a decrease. By focusing on the former patients and ignoring the latter, we convert statistical noise into a clinical “disease.”

(2) do creatinine bumps reflect genuine renal injury?
Let's imagine for a moment that contrast dye does cause a transient elevation in creatinine. Creatinine is an inert molecule, with no physiological effect. The next question is whether small elevations in creatinine actually reflect genuine kidney injury (or whether they might simply reflect transient reductions in creatinine secretion). It's crucial to realize that some drugs cause transient reductions in creatinine secretion without actually damaging the kidneys – such drugs are termed pseudo-nephrotoxins.
There is no evidence in the literature that small increases in creatinine sometimes seen following contrast dye administration reflect actual kidney injury. Studies using renal biomarkers have found no signal of renal injury following contrast dye exposure – even in patients with elevated creatinine levels meeting the definition of “contrast nephropathy.”(25773936) Thus, the definition of “contrast nephropathy” in terms of small creatinine bumps is flawed, as these elevations don't seem to reflect any genuine renal injury.
(3) what is the impact on patient-oriented clinical endpoints?
Let's be honest though – what everyone worries about most is dialysis. We're not really worried about causing a small bump in the patient's creatinine, or even causing transient renal injury. We're worried about a severe renal insult which would require dialysis. And, of course, we worry about mortality.
Virtually every study has found no evidence that contrast increases the risk of dialysis or death.(23319662, 28131489, 28811122, 25203000, 26250726, 26001222) One study focusing on ICU patients did find that contrast correlated with an increased likelihood of requiring dialysis among patients with a GFR<45 ml/min. Bizarrely, this same study found no signal that contrast correlated with increased creatinine levels. How could contrast dye increase the risk of dialysis, without affecting renal function? The answer might be an increased rate of dialysis due to the volume overload associated with contrast dye (which may largely reflect fluid given to prevent “contrast nephropathy”).(28213620)
 bottom line: no coherent evidence of harm
bottom line: no coherent evidence of harm
Despite decades of searching and literally thousands of publications, there is no coherent evidence that modern contrast dyes cause clinically meaningful harm. The vast majority of recent publications suggest that modern contrast dyes are safe. A few publications raise the possibility of harm, but these studies are overall inconsistent (e.g., increased risk of dialysis without increased risk of kidney injury).
Unfortunately, we will never be able to exclude the possibility that contrast dye is nephrotoxic with 100% certainty (this is methodologically impossible, because it would require a massive prospective RCT). However, the best available evidence indicates that contrast dye is safe. If contrast dye were nephrotoxic, then it would have to be an extremely weak nephrotoxin of no real clinical significance.
Overall, given the massive amount of study which has been spent on this issue, it's highly reassuring that no definitive evidence of harm has been found. The renal effects of contrast dye have probably been more intensely investigated than the renal effect of any other drug or substance in medical history.
 Clinicians are often tasked with balancing the risk-vs-benefit of the administration of IV contrast for CT scanning. Currently, this calculation would seem to be as follows:
Clinicians are often tasked with balancing the risk-vs-benefit of the administration of IV contrast for CT scanning. Currently, this calculation would seem to be as follows:
- Risk of using contrast dye: There is no high-quality evidence that this risk exists.
- Benefit of using contrast dye: This is often quite real (although it will certainly vary, depending on the clinical scenario).
From an evidentiary standpoint, avoidance of contrast dye is difficult to justify. Physicians are often risk-averse, as we certainly want to avoid causing harm. However, the best available evidence suggests that our patients will benefit the most if we don't shy away from using contrast dye in scenarios where it is indicated.
“Renalism” refers to the avoidance of contrast dye in patients with renal dysfunction, causing a failure to perform important studies and leading to harm.(25318756) In the current era of improved contrast dyes, renalism poses a greater risk to our patients than does “contrast nephropathy.”
Hinson et al. sums this up well in their conclusions following a trial involving septic patients at John Hopkins (CM=contrast medium):(30798098)

Given how much we worry about contrast nephropathy, you might think that contrast dye is the only potentially nephrotoxic substance in the hospital. In fact, contrast dye is probably among the least nephrotoxic things that we prescribe. The following list includes commonly used drugs which are definitely nephrotoxic:
known nephrotoxins commonly encountered in critical care:
- Antibiotics
- Vancomycin
- Aminoglycosides
- Amphotericin
- Antivirals: Acyclovir, ganciclovir
- ACE-inhibitors, Angiotensin receptor blockers (ARBs)
- NSAIDs
- Mannitol
- Normal saline (in large volumes)
We worry a lot about contrast nephropathy because it has its own special name. Meanwhile, we often don't think much about other drugs, which are proven nephrotoxins. This is entirely illogical.

Avoiding nephrotoxins among critically ill patients is obviously important. Our efforts along this vein should be aimed at drugs which are known nephrotoxins. We need to stop worrying about IV contrast dye and focus more on drugs which are actually causing harm. We're wasting our time chasing a ghost, while true card-carrying nephrotoxins often pass by without much attention.
Renal injury can occur following intra-arterial procedures (e.g. cardiac catheterization). It's unclear why this occurs, with possible causes including the following:
- Patients are in heart failure or cardiogenic shock with high risk of renal failure (regardless of any intervention). The occurrence of renal failure following catheterization may merely represent association, not causation.
- Dislodgement of cholesterol plaques with embolization to the kidneys.
- Other periprocedural complications (e.g. arrhythmia, hemorrhage).
- Use of intra-aortic balloon pumps (which may occlude renal blood flow when positioned incorrectly).(20837932)
- Direct effect of contrast dye.
This is hard to sort out because it's impossible to perform a non-contrast cardiac catheterization. Therefore, it's even harder to investigate this topic than it is to investigate IV contrast for CT scans.
No clear statement can be made on this topic currently. Unlike CT scans, this issue is less ubiquitous among critically ill patients. It may be best to defer management of this issue to interventional cardiologists (who will invariably be involved in the management of any patient going to the cardiac catheterization lab).

Follow us on iTunes
The Podcast Episode
Want to Download the Episode?
Right Click Here and Choose Save-As
To keep this page small and fast, questions & discussion about this post can be found on another page here.

- Failing to use contrast for CT scans due to fear of nephropathy, leading to suboptimal imaging studies which impair subsequent management (a.k.a. Renalism).
- Delaying scans in critically ill patients while awaiting “clearance” to use IV contrast.
- Administration of additional fluid to prevent “contrast nephropathy” for CT scans in critically ill patients who have already been volume resuscitated (if the patient is already euvolemic, additional fluid may provoke volume overload, which itself is nephrotoxic!).
Key articles to cite supporting the use of IV contrast dye 🔑
- If you need some solid peer-reviewed articles to drop into the chart:
- Aycock RD, Westafer LM, Boxen JL et al. Acute Kidney Injury after CT: A meta-analysis. Annals of Emergency Medicine 2018.(28811122) Exhaustive, modern literature review in the Annals showing no difference in acute kidney injury, mortality, or dialysis.
- Hinson JS, Jalbout NA, Ehmann MR et al. Acute kidney injury following contrast media administration in the septic patient: A retrospective propensity-matched analysis. Journal of Critical Care 2019.(28131489) Large study evaluating patients presenting to John Hopkins with suspected sepsis. No effect was detected from contrast dye, even among patients with GFR<30 ml/min.
- Ehrmann S, Aronson D, Hinson JS. Contrast-associated acute kidney injury is a myth: Yes. Intensive Care Medicine 2017 (29242967)
Guide to emoji hyperlinks 
= Link to online calculator.
= Link to Medscape monograph about a drug.
= Link to IBCC section about a drug.
= Link to IBCC section covering that topic.
= Link to FOAMed site with related information.
= Link to supplemental media.
References
- 13217726 BARTELS ED, BRUN GC, GAMMELTOFT A, GJØRUP PA. Acute anuria following intravenous pyelography in a patient with myelomatosis. Acta Med Scand. 1954;150(4):297-302. doi: 10.1111/j.0954-6820.1954.tb18632.x [PubMed]
- 17317065 Sandstede JJ, Roth A, Machann W, Kaupert C, Hahn D. Evaluation of the nephrotoxicity of iodixanol in patients with predisposing factors to contrast medium induced nephropathy referred for contrast enhanced computed tomography. Eur J Radiol. 2007 Jul;63(1):120-3. doi: 10.1016/j.ejrad.2007.01.021 [PubMed]
- 20651198 Ng CS, Shaw AD, Bell CS, Samuels JA. Effect of IV contrast medium on renal function in oncologic patients undergoing CT in ICU. AJR Am J Roentgenol. 2010 Aug;195(2):414-22. doi: 10.2214/AJR.09.4150 [PubMed]
- 20707658 Lencioni R, Fattori R, Morana G, Stacul F. Contrast-induced nephropathy in patients undergoing computed tomography (CONNECT) – a clinical problem in daily practice? A multicenter observational study. Acta Radiol. 2010 Sep;51(7):741-50. doi: 10.3109/02841851.2010.495350 [PubMed]
- 20837932 Rastan AJ, Tillmann E, Subramanian S, Lehmkuhl L, Funkat AK, Leontyev S, Doenst T, Walther T, Gutberlet M, Mohr FW. Visceral arterial compromise during intra-aortic balloon counterpulsation therapy. Circulation. 2010 Sep 14;122(11 Suppl):S92-9. doi: 10.1161/CIRCULATIONAHA.109.929810 [PubMed]
- 23319662 McDonald JS, McDonald RJ, Comin J, Williamson EE, Katzberg RW, Murad MH, Kallmes DF. Frequency of acute kidney injury following intravenous contrast medium administration: a systematic review and meta-analysis. Radiology. 2013 Apr;267(1):119-28. doi: 10.1148/radiol.12121460 [PubMed]
- 23360742 McDonald RJ, McDonald JS, Bida JP, Carter RE, Fleming CJ, Misra S, Williamson EE, Kallmes DF. Intravenous contrast material-induced nephropathy: causal or coincident phenomenon? Radiology. 2013 Apr;267(1):106-18. doi: 10.1148/radiol.12121823. Epub 2013 Jan 29. Erratum in: Radiology. 2016 Jan;278(1):306 [PubMed]
- 24475854 McDonald JS, McDonald RJ, Carter RE, Katzberg RW, Kallmes DF, Williamson EE. Risk of intravenous contrast material-mediated acute kidney injury: a propensity score-matched study stratified by baseline-estimated glomerular filtration rate. Radiology. 2014 Apr;271(1):65-73. doi: 10.1148/radiol.13130775 [PubMed]
- 24656402 Azzouz M, Rømsing J, Thomsen HS. Fluctuations in eGFR in relation to unenhanced and enhanced MRI and CT outpatients. Eur J Radiol. 2014 Jun;83(6):886-892. doi: 10.1016/j.ejrad.2014.02.014 [PubMed]
- 25183538 Schmalfuss CM, Woodard PK, Gitter MJ, Jadhav MP, Bellinger RL, Rose SC, Bavry AA. Incidence of acute kidney injury after intravenous administration of iodixanol for computed tomographic angiography. Int J Cardiol. 2014 Dec 20;177(3):1129-30. doi: 10.1016/j.ijcard.2014.08.054 [PubMed]
- 25203000 McDonald RJ, McDonald JS, Carter RE, Hartman RP, Katzberg RW, Kallmes DF, Williamson EE. Intravenous contrast material exposure is not an independent risk factor for dialysis or mortality. Radiology. 2014 Dec;273(3):714-25. doi: 10.1148/radiol.14132418 [PubMed]
- 25318756 Weisbord SD. AKI and medical care after coronary angiography: renalism revisited. Clin J Am Soc Nephrol. 2014 Nov 7;9(11):1823-5. doi: 10.2215/CJN.09430914 [PubMed]
- 25773936 Kooiman J, van de Peppel WR, Sijpkens YW, Brulez HF, de Vries PM, Nicolaie MA, Putter H, Huisman MV, van der Kooij W, van Kooten C, Rabelink TJ. No increase in Kidney Injury Molecule-1 and Neutrophil Gelatinase-Associated Lipocalin excretion following intravenous contrast enhanced-CT. Eur Radiol. 2015 Jul;25(7):1926-34. doi: 10.1007/s00330-015-3624-4 [PubMed]
- 26001222 Garfinkle MA, Stewart S, Basi R. Incidence of CT Contrast Agent-Induced Nephropathy: Toward a More Accurate Estimation. AJR Am J Roentgenol. 2015 Jun;204(6):1146-51. doi: 10.2214/AJR.14.13761 [PubMed]
- 26250726 McDonald JS, McDonald RJ, Lieske JC, Carter RE, Katzberg RW, Williamson EE, Kallmes DF. Risk of Acute Kidney Injury, Dialysis, and Mortality in Patients With Chronic Kidney Disease After Intravenous Contrast Material Exposure. Mayo Clin Proc. 2015 Aug;90(8):1046-53. doi: 10.1016/j.mayocp.2015.05.016 [PubMed]
- 28131489 Hinson JS, Ehmann MR, Fine DM, Fishman EK, Toerper MF, Rothman RE, Klein EY. Risk of Acute Kidney Injury After Intravenous Contrast Media Administration. Ann Emerg Med. 2017 May;69(5):577-586.e4. doi: 10.1016/j.annemergmed.2016.11.021 [PubMed]
- 28197679 Ehrmann S, Quartin A, Hobbs BP, Robert-Edan V, Cely C, Bell C, Lyons G, Pham T, Schein R, Geng Y, Lakhal K, Ng CS. Contrast-associated acute kidney injury in the critically ill: systematic review and Bayesian meta-analysis. Intensive Care Med. 2017 Jun;43(6):785-794. doi: 10.1007/s00134-017-4700-9 [PubMed]
- 28213620 McDonald JS, McDonald RJ, Williamson EE, Kallmes DF, Kashani K. Post-contrast acute kidney injury in intensive care unit patients: a propensity score-adjusted study. Intensive Care Med. 2017 Jun;43(6):774-784. doi: 10.1007/s00134-017-4699-y [PubMed]
- 28811122 Aycock RD, Westafer LM, Boxen JL, Majlesi N, Schoenfeld EM, Bannuru RR. Acute Kidney Injury After Computed Tomography: A Meta-analysis. Ann Emerg Med. 2018 Jan;71(1):44-53.e4. doi: 10.1016/j.annemergmed.2017.06.041 [PubMed]
- 29242967 Ehrmann S, Aronson D, Hinson JS. Contrast-associated acute kidney injury is a myth: Yes. Intensive Care Med. 2018 Jan;44(1):104-106. doi: 10.1007/s00134-017-4950-6 [PubMed]
- 30480553 Gorelik Y, Yaseen H, Heyman SN, Khamaisi M. Negligible Risk of Acute Renal Failure Among Hospitalized Patients After Contrast-Enhanced Imaging With Iodinated Versus Gadolinium-Based Agents. Invest Radiol. 2019 May;54(5):312-318. doi: 10.1097/RLI.0000000000000534 [PubMed]
- 30798098 Hinson JS, Al Jalbout N, Ehmann MR, Klein EY. Acute kidney injury following contrast media administration in the septic patient: A retrospective propensity-matched analysis. J Crit Care. 2019 Jun;51:111-116. doi: 10.1016/j.jcrc.2019.02.003 [PubMed]


