Happy Solstice!
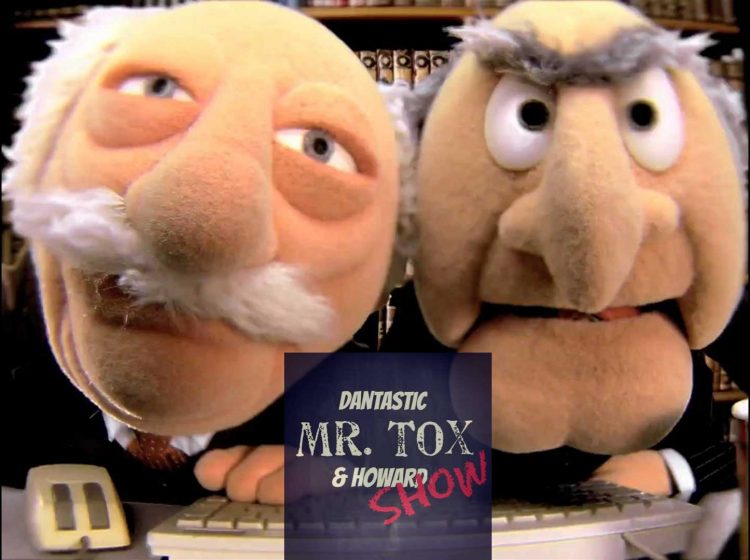
A delightful and hilarious toxicology podcast started up a few months ago, the Dantastic Mr. Tox & Howard Show. I managed to get the hosts on the line to talk some tox.
Howard Greller (@heshiegreshie)
Dr. Greller is EM and toxicology out of St. Barnabas in NYC

Dan Rusyniak (@drusyniak)
Dr. Rusyniak is EM and toxicology at Indiana University

Opioids
Intralipids
Calcium Channel Blocker Overdose
The Santa Beard
Additional New Information
More on EMCrit
- Approach to the critically ill poisoned patient(Opens in a new browser tab)
- Podcast 059 – Bath Salts with Leon Gussow(Opens in a new browser tab)
- Podcast 122 – Cardiac Arrest after the Toxicology of Smoke Inhalation with Lewis Nelson(Opens in a new browser tab)
- EMCrit 225 – Tox(&Hound)idromes with Howard & Dan
Additional Resources
You Need an EMCrit Membership to see this content. Login here if you already have one.
- EMCrit 373 – Mike Weinstock with another Critical Care Bounceback: “Asymptomatic Hypertension” - April 18, 2024
- EMCrit Wee – Ross Prager on 10 Heuristics for the New ICU Attending - April 13, 2024
- EMCrit 372 – FoundStab Intubation SOP - April 5, 2024

Great discussion! Some questions and points: 1) Is Dan and Howard’s reluctance to use lipids in CCB overdoses based on the availability of ECMO as an alternative? What if ECMO was not an option? 2) The discussion of decontamination in CCB overdose was a little vague. What would Dan and Howard suggest considering: multi-dose activated charcoal? whole bowel irrigation? gastric lavage????? Do they really believe that the potential (unproven) benefits are worth the risks. (I leave out single-dose charcoal with is probably safe in an alert cooperative patient.) 3) Do your guests see any role for bedside echo (LV squeeze,… Read more »
Leon, great questions (as always). My reluctance is based on my access to ECMO. Also, anecdotally, I have seen little benefit. The LogP’s of the three CCBs we are likely to see include Verapamil (5.4), Diltiazem (2.73) and Amlodipine (1.6). Based on this the most benefit would be expected in verapmil and the worst in amlodipine. I would consider it in a verapamil OD at an outside hospital. I am not opposed to trying it in the others but since we have ECMO would go to that sooner in these OD’s. For the second question on decontamination I suspect Howard… Read more »
Hi Leon! Thanks for the questions. My brief responses… I don’t have ECMO available in any form and would have to transfer a patient. I’m willing to try lipid, but don’t think that at least in the pig models (Bania and Chu) that it works so well. Plus the arguments made by Dr Weinberg in the podcast about timing and route. I’m a believer in decon and think that I give both charcoal and would WBI in bad cases. I know that there isn’t good data, but I think that some degree of common sense must prevail in serious poisoning.… Read more »
Howard: I think common sense could just as well argue against decontamination. If the patient is stable and not yet symptomatic, either they will deteriorate or they did not take a significant overdose. If the latter, they do not need decontamination. If the latter and they receive WBI, the treating physician might soon be faced with a hypotensive patient with a gut full of polyethylene glycol. It does not seem to me likely that one could often use WBI to transform a serious case into one that is benign. I’d have no problem with giving a stable cooperative patient a… Read more »
Hence the title of this episode. Can parse this in many ways. But I don’t think that we’ve ever been able to study this appropriately and would be very difficult to. To paraphrase one of my favorite mushroom sayings:
Falling in love is like eating a poisonous mushroom (a suspected CCB overdose). You never know it’s the real thing until it’s too late….