by Casey Albin, MD & Neha Dangayach, MD
Intro
About ~800K people have a stroke in the US every year (1 person every 40 seconds) and stroke is a leading cause of serious long-term disability (PMID: 31992061). But prior to ~2015, outside of trials, the acute ischemic stroke patient either arrived within 4.5 hours and got tPA or they got supportive care. And, unfortunately, very few patients arrive within the 4.5 hour time window.
Things are dramatically different now. The endovascular era in stroke care has revolutionized care for patients with large vessel occlusions (LVO) – which is the subgroup of patients that before the reperfusion era accounted for the highest stroke morbidity and mortality. There is now effective treatment for those who present within 24 hours.
If nothing else, we hope this post impresses on you the importance of treating ischemic stroke like an MI or any other intervenable condition.
TIME IS BRAIN, and with 1.9 million neurons being lost with every minute of delay, it is important to have acute ischemic stroke codes down cold (PMID: 16339467).
This post reviews the basics of stroke care including some pearls about neuroimaging and then reviews some of the major trials of 2021; the results of which are already transforming stroke care now.
Sections
- Stroke Care from Ambulance Bay to Head CT
- Neuroimaging in Stroke
- Thrombolysis Treatment (tPA and TNK)
- Clinical Worsening and tPA Related Complications
- Summary and Rapid Reference
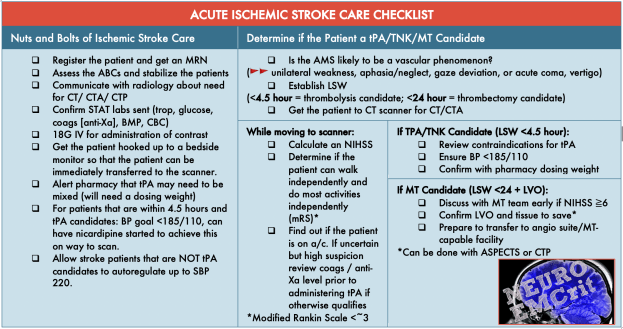
Care for a patient that is within 24 hours of last seen well (LSW) requires expedited ED care:

You will work with the neurologist or tele-neurologist to determine:

Stroke is the sudden onset of focal neurologic deficits due to a vascular event. “Is this a vascular syndrome?” is a question that clearly matters. The number of patients that show up with altered mental status is far greater than acute stroke. The key in stroke care is to recognize stroke syndromes.

The NIH Stroke Score (or here) has become an objective way to communicate stroke severity. But, it can be a hassle to calculate, and the difference between 10 and 12 has very little clinical significance. The NIHSS is weighted heavily on language and does a poor job of identifying deficits due to a vascular event in the posterior circulation.
It is more effective to recognize that a patient has a syndrome (like the ones above) and then determine what treatment the patient may qualify for.
- All patients with a function-limiting deficit (even if a low NIHSS) should be considered for thrombolysis if LSW <4.5 hours ago.
- Patients who present after 4.5 hours have historically been excluded from receiving thrombolysis, this is an active area of research, which we cover at the end of the post.
- Patients who present after 4.5 hours but within 24 hours, AND have a large vessel occlusion (LVO) may be candidates for mechanical thrombectomy/endovascular therapy (MT/EVT). MT will be extensively discussed in Part II of this post. (Stay tuned for details about the specific imaging, inclusion/exclusion criteria, and work flows for these patients!)
For now, for now it's important to recognize that patients with large vessel occlusions present with recognizable syndromes.

Thus, the patient that presents with:
- A left gaze preference
- Subtle drift in the right upper extremity
- Mild facial weakness on the right
- Mild-moderate aphasia
(a very modest NIHSS 4) merits a STAT CTA as this is an MCA syndrome and may be caused by a well collateralized M1 occlusion that has a high potential for neurologic decline and might still benefit from endovascular therapy.

Non-Contrast Head CT AND CT Angiography Head and Neck are the backbone of acute stroke management
The NCHCT is useful to:

The NCHCT is also used to determine the Alberta Stroke Program Early CT Score (ASPECTS), which scores the degree of damage already done. A point is subtracted for each area of early ischemic damage.

For example:

Above, the labeled segments in red demonstrate blurring of the normal gray-white architecture which is consistent with early ischemic changes. The unlabeled image is just to have an unobscured comparison with the ischemic tissue outlined.
From this cut the patient loses 4 points.
Scrolling up a few sections, M5 has also lost normal architecture and there is loss of the sulci. At M4 and M6 there is still some gray-white differentiation.

This scan is an ASPECT score of 5. We'll return to ASPECTS; it becomes very important in the determination of candidacy for thrombectomy.
The Head & Neck CT Angiogram
- Determines if there is a large vessel occlusion (anterior circulation = MCA M1 segment or ICA occlusion; posterior circulation = basilar)
- Determines the degree of collateral circulation
- Gives insight into the etiology of stroke (intracranial atherosclerosis, artery-to-artery embolism, plaque in the ICA or aortic arch, carotid web, etc)
If it turns out you scan the patient and find a bleed, no worries, the CTA is helpful then in ruling out a vascular malformation and evaluating for a spot sign (which may portend early worsening and hemorrhage expansion).
Does every suspected acute stroke need the CTA?
- If you have a true stroke syndrome like those above (including acute coma/disorder of consciousness without a clear etiology – basilar issue!), the CTA is important in determining management and etiology.
- Real world data from implementing a “CTA-for-All” policy for acute ischemic strokes within 24 hours of LSW resulted in higher rate of detection of LVO and shorter times to mechanical thrombectomy (PMID: 31684848)
- But remember, the only imaging you need to start thrombolysis is a NCHCT showing no hemorrhage. If the patient is thrombolysis eligible, you can start tPA or TNK while obtaining vessel imaging.
- Practically speaking, if the clinical suspicion is high, and the resources are available, neurology and pharmacy can accompany the patient to the scanner, mix tPA, recheck blood pressure and administer thrombolysis as soon as the HCT rules out a bleed. Then, while tPA is running proceed with CTA head and neck.
Currently Alteplase, a recombinant tissue plasminogen activator, abbreviated tPA is the only FDA approved thrombolytic for acute ischemic stroke. Tenecteplase (abbreviated TNK) is a genetically modified recombinant tissue-type plasminogen activator that is rapidly gaining more evidence in acute stroke treatment. The advantages of TNK are that it is more selective, has a longer half-life, and can be administered as a single bolus dose. More on the data, below.
Thrombolysis benefit:

- The benefit of tPA (and TNK) is time dependent. Although trials report on the improvement “within 3 hours” (NINDS, PMID: 7477192) or “within 4.5 hours” (ECASS III, PMID: 18815396) the reality is that the sooner thrombolysis is administered the better
- If a patient presents within 1 hour LSW there should be the same urgency to get tPA/TNK as if they are coming in right before the 4.5 hour cut off. You do NOT have time just because the patient is well within the window.
- It is important to remember that the NINDS data (PMID: 7477192) looked at the outcomes at 90 days using a crude metric (the modified Rankin Scores) and reported the relative increase in patients that had either “minimal or no disability” which made the effect of tPA seem modest (11-13% absolute increase).
- However, while patients would like to end up in the dichomized “good” category, this underestimates the treatment effect of tPA – ie that even if a patient doesn’t end up in the “good” group, they may still be better than they would have been.
- When you use nonbinary outcomes, the estimated NNT for 1 additional patient to have a better outcome by 1 or more grades on the mRS is 3.1 (CI 2.6-3.6).
- Meaning that for every 100 patients treated with tPA ~32 have a better outcome than when they are not treated and only 3 people in 100 are worsened by tPA. (PMID: 15262737) See image above ⬆️ (PMID: 29222229)
Tenecteplase (TNK) data:
- Five RCTs have been done for TNK. The first three trials included small numbers of patients and the pooled analysis demonstrated no significant differences in clinical outcomes or safety (PMID: 27048693). In EXTEND-IA TNK (PMID: 29694815) TNK demonstrated improved efficacy in vessel recanalization for a small amount of patients at a dose of 0.25mg/kg up to 25mg
- NOR-TEST compared doses of 0.4mg/kg and 0.25mg/kg, but the trial had a high number of stroke mimics and low severity strokes (PMID: 28780236).
- An RCT (ATTEST-2) for general use of TNK in non-LVO patients is underway with the 0.25mg/kg dose. However, already real world experience has demonstrated faster door-to-needle times with TNK using the 0.25mg/kg up to 25mg dose.
- If you do practice at a center using TNK, note that packing may reflect dosing for the myocardial infarction indication. Do not use the MI dosing.
Summary of the two thrombolytics:

Who Can't Get Thrombolysis?
The trials for tPA (NINDS and ECASSIII) had many exclusions. These that are now part of AHA/ASA guidelines (PMID: 31662037) and are applied to TNK by extension.
Broadly speaking there are 3 categories of disqualifications:

*Note these are trial exclusions, each case should be discussed on a case-by-case scenario, especially regarding the relative contraindications. BP>185/110 should be promptly addressed with antihypertensives so that the patient falls into a range where they qualify.
Thrombolysis is considered a procedure at many hospitals, and most have protocols about the need for consent/assent. Know your hospital's policy and make sure to document consent, if required to do so.

What about thrombolysis when LSW is not precisely known?
- Many strokes are wake up strokes where they patient may have had recent symptom onset but it cannot be proven by history.
- WAKE-UP was stopped early for funding reasons but investigated the effect of tPA when patients had a MRI proven DWI restriction (acute stroke), but no FLAIR changes on MRI (no evidence of subacute timing). In this unique situation, alteplase did modestly improve outcomes. The median score on the mRS at 90 days was 1 (no significant disability) in the alteplase group and 2 (slight disability) in the placebo group. (PMID: 29766770)
- The Phase II Chablis trial was just presented at #ISC22 International Stroke Conference. Patients were enrolled to receive TNK if they had perfusion mismatch (meaning the penumbra tissue at risk was larger than the core infarct, more on this when we talk about selection for MT) and a last seen well within 24 hours. This was a dose finding trial comparing two TNK dose strategies. Symptomatic ICH was low in both doses (~10%) in both dose groups. and 49% of patients in the 0.32mg/kg group achieved an mRS of 0-1 (excellent outcomes).
- This is still an active area of research, but soon we may be able to use perfusion imaging to select wake up stroke patients for thrombolytic treatment.
In patients treated with thrombolytics, the most feared complication is a tPA related hemorrhage. But, hemorrhage is only one reason that a patient may worsen during their acute stroke presentation.

When a patient acutely worsens after thrombolytics, the next step it to obtain a STAT HCT. Any thrombolytic-related bleed should follow the following algorithm from AHA/ASA. (PMID: 31662037)

If the head CT does not show a bleed, then it is important to determine if the patient has a blood pressure dependent exam. This can be accomplished by lowering the head of the bed and bolusing fluids and/or administering pressors. The goal is usually to achieving the last MAP documented before the patient had worsened.
If there is no difference after these adjustments, then other etiologies of worsening should be considered.
Don't worry all the nuts and bolts of mechanical thrombectomy will be covered in Part 2.
- EMCrit 336 – Team NeuroEMCrit's Critical Neuro Cases – Part 2 - November 3, 2022
- NeuroEMCrit – Team NeuroEMCrit's H&R Conference Talk, Part 1 - October 3, 2022
- NeuroEMCrit – The Perils of the ICH Score - August 1, 2022

This is one of the best posts on this site in recent memory. And only partially because it helps justify my disdain for NIHSS!!
Thank you!
Excellent post, well done!
thank you!
great post!
Thank you Marisa!!!
Thank you , Casey and Neha… excellent , detailed review. Thank you, Scott , for bringing them onto the team. one of the most difficult cases for me is the “dizzy” or vertiginous patient. It seems that that is the one who might be sent to the waiting room without the “stroke alert” called. It’s just a much tougher nut to crack. Anyone can call a hemiplegic aphasic patient at the door or pre-hospital. The posterior strokes scare the heck out of me. I just need to get better. (yes, Scott just did a super cool blog (#316) with Peter… Read more »
Thank you Thomas! I’d never heard of the VAN score, but this is great. Weakness+ Visual disturbance, aphasia, or neglect. I really like this as a simple way to triage patients and does capture some of the posterior circulation issues with the double vision / field cut… can still think of some posterior circulation that would be missed but if it were a basilar thrombosis, NIHSS would be >6 — the other criteria. for others interested linked here. thanks for sharing!!
Thank you, Casey!! Very kind of you. We brought it up briefly at an RLA (resus leadership academy (see in margin below… highly recommend it); Scott said he CTA’s every patient because it picked up cervical vascular pathology like dissections.
I learned about VAN from an Evie Marcolini pod… she’s super cool as well.
thank you!!
tom
Muy interesante
I contacted this herbal doctor (Robinson_buckler11) yahoo .com, to know how he can help me and he told me never to worry that he will help me with his natural herbal medicine! after 2 days of contacting him, he told me that the herbs was ready and he sent it to me via courier and it got to me! i used the medicine as he instructed me and i was cured from herpes! its really like a dream, i’m so happy! if you need his help______________________________
Really enjoyed this post – well written- thank you
This was an excellent article! Digestible information that was clearly and thoroughly explained. Thank you!