I've been waiting for this one for a long time. I got to interview Dr. Stephen Bernard on the topic of post-cardiac arrest care.
Professor Stephen Bernard
 Professor Stephen Bernard is a senior intensivist at the Alfred Hospital and Director of Intensive Care at Knox Private Hospital in Victoria, Australia. He is also Medical Advisor to Ambulance Victoria. Dr. Bernard was the lead author on one of the original establishing studies for post-arrest temperature management.
Professor Stephen Bernard is a senior intensivist at the Alfred Hospital and Director of Intensive Care at Knox Private Hospital in Victoria, Australia. He is also Medical Advisor to Ambulance Victoria. Dr. Bernard was the lead author on one of the original establishing studies for post-arrest temperature management.
My discussion with Dr. Bernard was based on a talk he gave at the Australasian College for Emergency Medicine
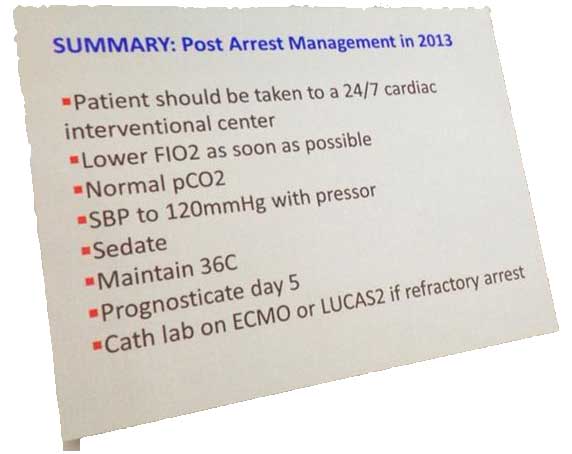
Maintain 36 C for 24 Hours
Dr. Bernard and the Alfred Hospital in Australia are moving to the protocol outlined in the TTM trial
Update 2023: now would like be normothermia
Is there anyone who still deserves to be cooled to 33 C?
Dr. Bernard feels patients that get intra-arrest cooling may still benefit until we have further trial results.
Neuro-Prognosticate as per the protocol in the Nielsen trial
Chris Nickson summarized the Neuro-Prognostication Protocol wonderfully
Time Zero Prognostication
It is tough. Unwitnessed asystole is probably one situation in which you can choose a palliative route if the situation otherwise supports it.
Pt should be taken to a 24/7 cardiac interventional center
This doesn't necessarily mean the patient needs to go to the lab immediately, they just need to be able to go when needed
Lower FiO2
Maintain an SpO2/SaO2 between 90-95%
Normal PaCO2
No hypocapnea, Perhaps slight hypercapnea
Tune in Next Week for Part II of the Interview
More on the TTM Trial
The Thoughts of Others
https://twitter.com/JAMyburgh/statuses/402940221630603264
https://twitter.com/JAMyburgh/statuses/403351251791781888
More from Steve can be found at the EDECMO Podcast Site
Additional New Information
More on EMCrit
Additional Resources
You Need an EMCrit Membership to see this content. Login here if you already have one.
- EMCrit 373 – Mike Weinstock with another Critical Care Bounceback: “Asymptomatic Hypertension” - April 18, 2024
- EMCrit Wee – Ross Prager on 10 Heuristics for the New ICU Attending - April 13, 2024
- EMCrit 372 – FoundStab Intubation SOP - April 5, 2024
Fantastic to have Steve Bernard share his wisdom on the EMCrit podcast.
He shows himself to be a true scholar and scientist, the way he has assimilated the findings of the TTM trial despite his long and ongoing interest in therapeutic hypothermia.
Steve, I salute you!
Chris
“Induced hypothermia does not have a role in any patient outside the context of a high-quality RCT.”
Woo, strong statement to digest.
And I have to respectfully disagree. In the TTM study they calculated a 90% power to find a difference of 20% in mortality. This was their primary outcome. I’m not sure why. The two original HACA studies (Benard & Holtzer) both found less than 20% differences in mortality. So even before the TTM study enrolls a single patient I expect them to find a null hypothesis. In TTM Nielsen did have secondary outcomes to look at intact Neurologic function. This is what we really care about and I’m not sure why it wasn’t the primary outcome. Bernard & Holtzer both… Read more »
Garreth, these excellent points have been raised by many and I would answer, but luckily one of the authors addressed these specifically in this excellent lecture: http://www.intensivecarenetwork.com/index.php/icn-activities/icn-podcasts/882-aneman-life-after-ttm
Why not titrate vaopressors to “Mean Arterial Pressure”, more reflecting organ perfusion compared tot systolic blood pressure?
I personally agree. I use a MAP of 80-100 as my goal.
Are there studies on post arrest survival in communities that have Organized 1-2minute response times to collapse some of which are cardiac arrest .
Is Vt VF higher when response is 1-2 minutes .